Health Social Workers in Promoting Mental Health Equity: Voice and Agency for the Marginalized
Chandramathi Ramaswamy, Bharathiar University
Revanth R, Bharathiar University
Jagadeesh R, Bharathiar University
Tamilarasu Sampath, Bharathiar University
F. X. Lovelina Little Flower, Bharathiar University
Abstract: Globally, 1 in 4 persons have mental health issues at some point in life. However, the mental health services are not easily available, accessible and affordable to all strata of the society with varying socio-economic and cultural backgrounds. In healthcare settings, social workers work in a context where a greater number of other professionals often have medical expertise rather than social science background which makes their job unique. Thus, health social workers have a crucial role in attaining health equity at mental health settings. This article primarily investigates the contemporary role of health social workers in pioneer mental health institutions of India. The study has two phases, the first phase adopts in-depth interview method with mental health social work practitioners using self-structured interview guide that highlights the role of health social workers, especially in establishing mental health equity by de-stigmatization, reducing the disparities, equal access, etc. Totally eight Health Social Workers participated in the study from, NIMHANS, JIPMER, Vazhikatti, and National Health Mission (Coimbatore), two from each institute respectively. Thematic analysis was performed and themes were generated from the qualitative data gathered. In the second phase, literatures were identified from SCOPUS, Google Scholar and Web of Science databases for mapping pertinent literatures on international health social workers in mental health settings. The results of the thematic analysis and the literatures from various sources were compiled to understand the aspects of health social workers in addressing marginalized identity, structural inequalities, cultural sensitivity, intersectionality and providing voice and agency to the marginalized in shaping the mental health policy and programs. Therefore, the article aims to identify and bridge the gaps in the roles of health social workers in attaining health equity within this context.
Keywords: Health equity; mental health; health social workers; marginalized identities; cultural sensitivity; mental health equity
1 Introduction:
Health equity refers to everyone having fair opportunity to attain full health potential without being disadvantaged by social, economic, demographic, or geographic stratifiers (Braveman, 2014). This encompasses not just access to quality and affordable healthcare but also addressing social determinants of health like education, housing, employment, transportation, and environmental influences that shape health outcomes (Peterson, A. et al., 2020). Mental health equity is integral to overall health equity but continues facing barriers like stigma, fragmented policy attention, and inadequate resource allocation (Compton, M. T., & Shim, R. S, 2020). These barriers disproportionately affect marginalized groups including communities of colour, indigenous people, LGBTQ populations, those facing homelessness, refugees, and persons with disabilities (Golden, S. 2022). Health social workers, with their focus on cultural competence, advocacy, empowerment, and centring communities in decisions impacting them, play vital roles in overcoming barriers to mental health equity (Stanhope V et al., 2015). Through multifaceted initiatives encompassing clinical services, coordination, health promotion, education, outreach, research, and policy reform, they can pave the way for transformative system changes that dismantle structural disparities and give everyone an equal chance for attaining mental wellness. However, additional investigation is warranted regarding best practices for health social workers in influencing mental health policy, forming cross-sector partnerships, employing community-based participatory methods, and undertaking advocacy efforts that capture intersectional needs of marginalized populations based on race, gender, socioeconomic status, and other demographic factors, in achieving Mental Health Equity.
1.1 Shortage in Mental Health Workforce:
India faces a critical scarcity of mental health practitioners, namely psychiatrists, which greatly hinders the provision of sufficient mental healthcare (Praharaj, S. et al, 2013; Kumar, P., 2018; Gupta, S., 2021). In India, the ratio of psychiatrists to the population is significantly low, standing at 0.3 per 100,000 inhabitants (Hariharan, S. et al, 2020). This figure falls much below the World Health Organization's recommended ratio of 1 psychiatrist per 100,000 individuals (Bishnoi, H. et al, 2017). This shortage also applies to child psychiatrists and mental health nurses, further worsening the lack of mental health knowledge and skills. The scarcity of mental health practitioners in India is exacerbated by various factors, like lack of adequate exposure and low interest among medical undergraduates that contribute to psychiatry not being a favoured specialisation. The ratios of mental health social workers are 0.033 per 100,000 people and 0.047 for psychologists (Bishnoi, H. et al, 2017). The ratios of these specialists are much lower than the global requirements. The scarcity of resources results in a treatment deficit of more than 70% for psychiatric diseases, underscoring the pressing necessity for remedies (Jayasankar, P. et al 2022). Enabling primary care physicians to handle psychiatric disorders could help address this deficiency. Moreover, the movement of mental health practitioners from poor and middle-income countries to countries such as the United Kingdom, United States, New Zealand, and Australia has an additional effect on the ratio of psychiatrists to the population in their countries of origin (Jenkins, R. et al, 2010). India's allocation of lesser than 2% of its yearly health budget to mental health fails to meet the standard of proportional spending, continues to perpetuate the existing difficulties (Center for Mental Health Law and Policy, 2023; Mahajan, P. et al, 2019). This suboptimal allocation may lead to insufficient and inadequate provision of mental health services. Low-income countries face similar inadequacies in mental health professionals compared to high-income ones, with a notable discrepancy in the number of registered psychiatrists, social workers, mental health nurses and clinical psychologists (Okechukwu, C. 2021). The Health Resources and Services Administration's (HRSA) National Centre for Health Workforce Analysis in United States, published a report in 2016 that predicts a deficit of about 10,000 full-time staff for mental health and substance use disorder (SUD) social workers and school counsellors. The convergence of these issues underscores the urgent requirement for initiatives, legislative reforms, and augmented funding in mental health to tackle the acute scarcity of mental health practitioners and deliver comprehensive care in India.
This article aims to explore the roles of health social workers in promoting mental health equity and map existing literature to identify evidence-informed recommendations on tangible steps they can take to advocate for the needs and preferences of disadvantaged communities in the contexts of research, practice, and policy. It further examines opportunities for them to collaborate with grassroots organizations and how health social workers shape people-centred mental healthcare that reduces gaps in accessibility, achieving equity, and policy inclusivity.
2 Method:
2.1 Objective and Research Question:
The broad objective that guides the article is to understand the role of health social workers working in various mental health settings in promoting mental health equity, and how they address the gaps of health equity differing from other healthcare professionals. The research questions framed by the researchers for the study are,
1. What is the role of health social workers in mental health setting and how do they differ from other healthcare professionals?
2. How health social workers address the mental health issues overcoming the social stigma and promote Mental Health Equity?
For addressing these research questions the study was conducted in two phases, in which first phase conducted in-depth interview with health social work practitioners and in the next phase, literatures were identified on international health social workers. These literatures were mapped with the themes generated from phase 1 and the results were discussed based on the questions framed.
2.2 Phase 1:
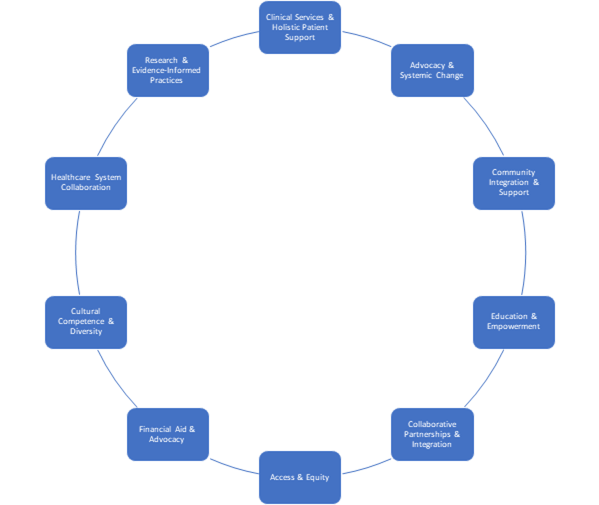
For understanding the roles performed, an in-depth interview was conducted among the health social workers working in top tier mental health institutions namely, NIMHANS, JIPMER, Vazhikatti, and National Health Mission (Coimbatore), two respondents from each institute were selected, totally eight health social workers participated in the phase 1 of the study. An interview guide composing questions related to the roles and responsibilities of the health social workers in the institute, how they see themselves different from other healthcare professionals, the problems they encountered from their clients due to social stigma, and how do they contribute in achieving mental health equity and what are the areas that has to be focused in future for betterment of mental health equity, was prepared. Thematic analysis using the Braun and Clarke six stages (Clarke, V., & Braun, V., 2017), was carried out for each question (Refer annexures, for the codes and themes generated for each question). The Codes were generated by the first and third author and the common themes were identified by the second author. Finally, all the authors rechecked the codes and themes, unanimously approved the themes like Clinical Services & Holistic Patient Support, Advocacy & Systemic Change, Community Integration & Support, Education & Empowerment, Collaborative Partnerships & Integration, Access & Equity, Financial Aid & Advocacy, Cultural Competence & Diversity, Healthcare, System Collaboration and Research & Evidence-Informed Practices (refer figure 1). These themes reflect the roles performed by the health social workers in mental health settings for achieving mental health equity.
2.3 Phase 2:
Literatures on international health social workers in mental health settings were identified from databases like Scopus, Web of Science and Google scholar. Combination of words like Health social worker, mental health social worker, and the themes generated from phase 1 of the study were used as keywords for identifying pertinent literatures. Initially, 632 literatures were identified, based on the inclusion and exclusion criteria (refer table 1), 267 literatures were found eligible for screening. The Title and Abstract of these 267 literatures were screened by the researchers and selected 96 articles eligible for full manuscript reading. First four authors reviewed 24 articles each. Finally, based on each author’s opinion on how well the article aligns with the questions framed for the study; 82 literatures were selected and the results were discussed based on the questions framed, combining the results obtained from phase 1 and phase 2.
Table 1: Inclusion and Exclusion criteria
|
Inclusion Criteria |
Exclusion Criteria |
|
Peer reviewed |
Preprints |
|
Open access |
Protocols |
|
Publication year from 1990 to 2023 |
Population other than Health Social Workers |
|
Should align with the objective of the study |
- |
Figure 1: Common Themes identified from the generated themes.
3 Results:
3.1 Social Workers in Mental Health:
In the landscape of mental health, social workers play multifaceted roles that encompass a spectrum of responsibilities (Feryn, N., 2021; Fairfax, C., & Feit, M., 2015). Their contributions span across various settings, each with its distinct focus yet interconnected in their commitment to fostering holistic well-being and health equity (Klos, L. et al, 2021; Weng, S, 2021). Let's delve into the integrated narrative that amalgamates the diverse themes delineating the roles and responsibilities of health social workers in mental health settings. They offer comprehensive healthcare support, through providing emotional, social, and practical support beyond medical issues to provide complete patient care (Dennelly, L., 2021; Bamford, T., 2011). They campaign for structural reform to improve patient access to and advocate for legislation and support vulnerable groups to improve health equity (Nazar, N., 2020). They coordinate all aspects of patient care by communicating with stakeholders and assisting doctors and patients in providing holistic care (Shanske, S. et al, 2012). Individualised care plans after rigorous assessments are also given by them using strategies customised for each patient, ensuring optimal results. In the realm of mental health settings, health social workers extend pivotal clinical services. They engage in therapeutic interventions, employing diverse modalities to support individuals coping with mental health challenges (Woerner, C., 2015; Francis, A., 2014). Through counselling and psychotherapy, they create a safe space for exploration, healing, and resilience-building (Booysen, P., & Staniforth, B., 2017; McLeod, J., & McLeod, J., 2015). These professionals adeptly navigate the complexities of case management (Okech, V., 2020; Denis, G., & Ellis, S., 2017). They coordinate services, advocating for their clients' needs within intricate systems (Sheehan, R., 2012). By orchestrating resources and support networks, they strive to enhance the quality of care and accessibility to essential services. One of their fundamental responsibilities lies in fostering awareness and empowerment through psycho-education (Pardasani, M., 2018). They disseminate crucial information about mental health, empowering individuals to comprehend their conditions, treatment options, and available support programs (Nazar, N., 2018). Social workers in mental health settings thrive in interdisciplinary collaborations (Noel, L., 2022; Jones, B., & Phillips, F., 2016). They bridge gaps between various stakeholders, ensuring a comprehensive approach to care by integrating perspectives from psychologists, psychiatrists, medical practitioners, and community resources. Their involvement in treatment planning encompasses a holistic approach, considering both therapeutic interventions and medication management (Winkelmann, G., 2016). They facilitate discussions, aiding clients in understanding treatment options while supporting adherence and management of prescribed medications (Jensen, C., 2004). Furthermore, Social workers champion community integration and reintegration (Rosenheck, R., 2012). They facilitate the transition of individuals back into their communities post-treatment, promoting acceptance, understanding, and support within their social milieu (Wilkinson, G. et al, 2017).
3.2 Health Social Workers Vs Other Healthcare professionals:
Health Social workers offer a unique blend of skills and perspectives that distinguish them from other healthcare professionals (Andrews, C. et al., 2013; Bergstrøm, C., 1979). The distinctive themes evolved from the analysis of the responses, define their approach and contributions revolve around patient-centred holistic care, comprehensive assessment, community integration, care coordination, crisis support, and policy advocacy. One of the fundamental differentiators of health social workers in mental health settings is their commitment to a patient-centred holistic approach, unlike some healthcare professionals who may focus primarily on medical interventions, health social workers adopt a holistic view, recognizing the interconnectedness of various aspects of an individual's life (Ashcroft, R.et al.,2017; Mann, C. et al., 2016; Berkman, B. et al., 1996). They consider not just the symptoms but also the social, environmental, and psychological factors influencing mental health, ensuring a more comprehensive understanding of the patient's needs. Advocacy and system navigation are integral components of a health social worker's role as they advocate for their clients, helping them navigate complex healthcare systems, access resources, and assert their rights (Mango, L., 2020). By bridging the gap between patients and services, health social workers empower individuals to navigate bureaucratic hurdles and access necessary care effectively (Faust, J. 2008; Chappell, N., 2008). Furthermore, mental health social workers excel in assessment beyond the medical lens but view the psycho-social aspects through social justice lens. While medical professionals primarily focus on diagnosing and treating illnesses, health social workers conduct comprehensive assessments that encompass not only clinical symptoms but also social determinants, cultural nuances, and environmental factors influencing mental health (Berkman, B. et al., 1990; Levy, C. 1985). This broader perspective allows for more tailored and effective interventions. Another defining aspect is their commitment to community integration and support (Yip, K., 2000). Health social workers recognize the significance of community in an individual's mental health journey. They facilitate connections to support groups, community resources, and social networks, fostering a sense of belonging and providing ongoing support outside clinical settings (Walter, A. et al., 2018). Care coordination and continuity are central to the role of mental health social workers. They collaborate with multidisciplinary teams, ensuring seamless coordination between various healthcare providers, social services, and community resources. This integrated approach enhances the quality of care and supports clients in maintaining continuity throughout their treatment journey. In times of crisis, the expertise of mental health social workers shines through their provision of emotional and crisis support by adopting to the principles of social work profession. They offer compassionate and immediate assistance, helping individuals navigate through challenging situations, mitigate crisis, and access necessary support services. Lastly, health social workers engage in policy advocacy and strive for systemic change and serve as voice and agency for the marginalized (Marshall-Lee et al., 2019; McLaughlin, A. 2009). They leverage their experiences and insights from frontline work to advocate for policy reforms that address systemic barriers, improve access to mental healthcare, and promote social justice (Hamer, H., et al., 2018). Among all one of the important aspects of health social workers are they offer a multifaceted approach that goes beyond traditional healthcare paradigms. Their emphasis on holistic care, advocacy, comprehensive assessment, community integration, care coordination, crisis support, and policy advocacy make them invaluable assets in promoting mental health and well-being within communities.
3.3 Addressing Mental health issues overcoming the Social Stigma
Social stigma has long plagued mental health in many societies (Corrigan, P. 1998). This stigma, ingrained in society, religion, and myths, has discouraged mental health treatment and discussion (Benbow, A. 2007; Corrigan, P et al., 2014). Cultural beliefs and misunderstandings have made mental health stigma a major concern for health social workers, especially in India with people with mental illness symptoms either doesn’t seek help from qualified professionals or in other case, seek help from traditional healers, shamans, etc. Culturally sensitive discussions, community leaders, and psycho-education should be employed to fight this. These programmes sought to reconcile cultural norms and mental health knowledge by emphasising mental health treatment like any other health issue. One such mental illness destigmatization initiative by NIMHANS is “Walking tour of NIMHANS” to break the stigma around mental illnesses. It is a unique educational effort to destigmatise misconceptions, reduce stigma, and increase public awareness about mental illnesses, related services and those who have experienced mental illnesses. Themes from the responses show that health social workers have to work together to overcome this stigma (Benbow, A., 2007). Creating friendly conditions and normalizing mental health treatment help eradicate stigma. Support groups helped people share their successful treatment stories, build community, and reduce mental health treatment hurdles. Addressing confidentiality concerns was key to easing privacy worries and spreading information on strict confidentiality laws and professional principles governing mental health care to reassure people about their privacy when seeking help. Psychoeducation changed attitudes towards seeking mental health help, reframing treatment as a brave step towards healing changed the narrative (Sagar-Ouriaghli et al., 2019; Jemalel, N. et al., 2016; Taylor-Rodgers, E., & Batterham, P. 2014). Health social workers in pioneer institutions majorly involve in tertiary care and knowledge imparting. They have conducted training of trainer sessions for the Primary health care workers, community health workers like ASHA workers, Anganwadi workers on the fundamental aspects of mental health, mental health first aid and de-stigmatization of mental illnesses. They also work on research projects for Ayushman Bharat Programme i.e. School health and wellness program where one male and one female teacher will be trained in the aspects of mental health and act as School’s Health and Wellness ambassador. Social attitudes changed by emphasizing mental health strength and educational workshops by psychiatrists eliminated psychiatric medicine myths. These sessions clarified concerns, explained medication management, and highlighted drugs' role in rehabilitation, helping people appreciate their importance and advantages. One of the primary strategies employed by health social workers involves extensive community involvement through outreach programs and health camps (Aviram, U., 1997). The Psychiatric department of JIPMER, Puducherry conducts regular Mental Health Camp in the outskirts of Puducherry to reach the rural population, as they are geographically marginalised in reception of mental health services. These initiatives aim to engage local communities directly, fostering understanding, empathy, and support for those affected by social stigma. By organizing events within the community, social workers create safe spaces for dialogue, education, and the exchange of ideas, breaking down barriers and prejudices. By recognizing the importance of education in combating stigma, they adopt diverse educational approaches, starting from integrating discussions about diversity and acceptance into school curricula to providing support and training in workplaces. Through workshops, seminars, and training sessions, they equip individuals with the knowledge and tools to challenge stereotypes, promote inclusivity, and create supportive environments. They also form partnerships with various entities, including governmental organizations, NGOs, healthcare providers, and community leaders (Levitt, A. et al., 2011). For instance NIMHANS collaborates with various states in implementation and training for District Mental Health Program (DMHP). They also collaborate with NGOs such as Chitta Sanjeevini Charitable Trust, an NGO supported by the Infosys Foundation, Lions Club International in Thirthahalli and Turuvekere to provide psychiatric medications, which are not available through the government sources, Samadhana Aptha Salaha Kendra run by Rajanna Achar Sarojamma trust, Nemmadi Kendra, etc. JIPMER also collaborates with NGOs like Trust for Youth and Child Leadership, Sathya Special School, etc., in Pondicherry. Together, they organize workshops, campaigns, and support groups aimed at fostering understanding, providing resources, and advocating for policy changes that promote inclusivity and reduce discrimination (Faust, J., 2008). One more advantages of collaborating with NGOs working with marginalised communities make mental health services available for the vulnerable. Harnessing the power of creative expression, health social workers utilize multimedia and cultural events as catalysts for initiating conversations around stigmatized issues. Through art, theatre, music, and other forms of expression, they create platforms for individuals to share their stories, challenge stereotypes, and evoke empathy (Igbaba, S., 2023). For instance, this year the department of Psychiatry, JIPMER, Puducherry celebrated World mental health day by conducting contest such as Slogan writing, Short film and e-poster on the theme “Mental health in Universal Human Right”. These creative endeavours serve as powerful tools in breaking down societal barriers and encouraging open dialogue.
3.4 Health Social Workers in Fostering Accessibility, Equity, and Policy Inclusivity – Promote Mental Health Equity:
In the pursuit of achieving health equity, health social workers play a pivotal role in addressing the systemic disparities that hinder access to mental health services (Hashimoto, H., & Kawakami, N., 2018; Bowen, E., & Walton, Q., 2015; Robinson, L. et al, 2012). Through a multifaceted approach, these professionals employ various strategies to bridge the gaps and ensure equitable access to mental health care for all individuals, regardless of socio-economic backgrounds (Hashimoto, H., & Kawakami, N., 2018). Equitable Access and Financial Support stand as foundational pillars in the mission to provide mental health services to marginalized communities (Shim, R., & Starks, S., 2021; Hailemariam, M. et al, 2016). Few such schemes are Rashtriya Arogya Nidhi, Ayushmaan Bharat, JIPMER Poor Fund that health social workers advocate patient and care taker and guide to get financial assistance. Through engaging in navigating complex fee structures, facilitating access to financial assistance, and advocating for government schemes that support mental health care and addressing socio-economic barriers, they with effective leadership strive to ensure that financial constraints do not inhibit individuals from accessing vital mental health resources (Hussain, A., & Ashcroft, R., 2020). Understanding the diverse backgrounds, languages, and geographical locations of individuals, health social workers initiate outreach programs, collaborate with NGOs, and engage communities to break down barriers (Gopalkrishnan, N., 2018; Shrivastava, S., 2014). By fostering inclusivity, they create a welcoming environment where individuals from all walks of life feel represented and understood in their mental health needs (Hamer, H. et al, 2018). Advocacy and Policy Influence form the backbone of efforts to effect substantial change, for policy alterations that prioritize mental health equity (Farrer, L. et al, 2015). They represent marginalized communities, amplify their voices in policy-making discussions, and raise awareness about the needs of these communities to ensure that policy changes reflect their realities (Saxena, A., & Chandrapal, S., 2021; Stewart, T., 2014). For instance, NIMHANS has made its significant contribution in National Disaster Management guidelines on Psycho-social and Mental Health support, inclusion of Persons with Mental illness in NREGA, etc. They educate policymakers, conduct research, and provide specialised workshops and awareness programmes to fill mental health care shortages. While, Collaboration with NGOs, educational institutions, and community organisations boosts their effect and promotes complete transformation. Technology, especially telemedicine, helps bring mental health services to disadvantaged groups (Bryant, L., et al, 2020; Orlowski, S. et al, 2017; Ramsey, A., & Montgomery, K., 2014). Tele-MANAS, a toll-free, 24/7 helpline number (14416) has been set up across the country allowing callers to select the language of choice for availing services. Service is also accessible with 1-800-91-4416 (Singh, A. et al, 2023; Ahmed et al, 2022; Sagar, R., & Singh, S. 2022). The calls would be routed to Tele-MANAS cells in the respective state and union territory operating with NIMHANS as nodal centre and JIPMER leading the Tele-MANAS unit for Puducherry. Additionally, integrating mental health care within existing healthcare systems provides a complete and seamless approach to mental health issues for everybody (Bensemann, C., & Watson, P., 2017). Their strategy emphasises empowerment and community support (Okech, V., et al, 2020). Health social workers create peer networks, customised courses, and skill-building programmes for marginalised communities (Fraher, E., et al, 2018). Lay counsellor training programs are conducted by NIMHANS to help spread the workforce in preliminary stages. NIMHANS provides Assisted home care (AHC) to needed and deserving patients with logistic difficulties (TNN, 2023, April 1). Thus, health social workers and the mental health institutions using their strategies empower accessibility, equity and policy inclusivity in mental health settings and promote mental health equity.
4 Scope for future research and conclusion:
Future mental health research bears potential and urgency across numerous topics that link human experiences and society institutions. Understanding marginalized identities is crucial in mental health services. Research should examine how race, ethnicity, gender, sexuality, and socioeconomic status affect mental health (Villatoro, A., et al., 2018). Researchers can create inclusive, effective interventions for various populations by recognising and comprehending these intersections. The study by Sawrikar, P. (2020) found that training in cultural competency enhances the quality of mental health services for ethnic minority clients by addressing racism, skin colour, and intersectionality. Access to mental health services remains unequal despite advances. An approach that acknowledges diversity and accommodates groups without discrimination is needed to reduce inequities in mental health services (Sussman, S., et al, 2020). Future studies should identify and overcome financial, geographical, cultural, and structural barriers to care. This requires identifying the gaps and offering innovative solutions to close the gap and provide equitable mental health support for everybody. Understanding trauma and its severe mental health effects is crucial for future research. Interventions must be responsive to varied trauma experiences. To help trauma survivors heal and recover, this entails trying new therapies, acknowledging cultural differences, and prioritising survivor-centred treatment. Mental health is where "prevention is better than cure" applies (Bhugra, D., & Till, A., 2013). Early mental health indicators and risk variables should be identified in future study to provide targeted prevention efforts. Early intervention programmes for various groups can reduce mental health issues and their impact on individuals and healthcare systems (Hooper, J., 2021; McGorry, P., & Mei, C., 2018). In conclusion, the themes identified in the study can help academics adapt mental health support to be egalitarian, inclusive, and sensitive to the different needs of individuals and communities worldwide to achieve mental health equity.
Author’s contribution
Conceptualization C.R, R.R, J.R; Methodology C.R, R.R, J.R; validation C.R, R.R, J.R; data analysis and data synthesis C.R, R.R, J.R.; writing- original draft preparation C.R, R.R, J.R writing- review and editing C.R, R.R, J.R, T.S; visualization C.R, supervision FX.L.LF, T.S. All authors have read and agreed to the published version of the manuscript.
Funding
This study did not receive any fund.
Informed consent statement / Ethical consideration
All participants gave verbal informed consent in accordance with the declaration of participation.
Data availability statement
Not applicable.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
On behalf of the research team, we wholeheartedly thank the mental health social work participants of the study from NIMHANS, JIPMER, Vazhikatti (Coimbatore), National Health Mission (Coimbatore). Their generous support, willingness to share insights, and dedication in providing comprehensive responses were instrumental in enriching our research. Their openness and valuable time devoted to answering our inquiries significantly contributed to the depth and quality of this study.
References:
Ahmed, T., Dumka, A., & Kotwal, A. (2022). Tele MANAS: India’s first 24X7 tele mental health helpline brings new hope for millions. Ind J Mental Health, 9(4), 403-406. https://indianmentalhealth.com/pdf/2022/vol9-issue4/14-Viewpoint-Article-2.pdf.
Andrews, C., Darnell, J., McBride, T., & Gehlert, S. (2013). Social work and implementation of the Affordable Care Act. Health & social work, 38 2, 67-71. DOI: 10.1093/hsw/hlt002
Ashcroft, R., Katwyk, T., & Hogarth, K. (2017). An Examination of the Holism Paradigm: A View of Social Work. Social Work in Public Health, 32, 461 - 474. https://doi.org/10.1080/19371918.2017.1360818.
Aviram, U. (1997). Social work in mental health: trends and issues. Social work in health care, 25(3), 1-9. https://doi.org/10.1300/J010V25N03_01.
Bamford, T. (2011). The Team Approach in Person-centred Health Care: The Social Work Perspective. the International Journal of Person-Centered Medicine, 1 (1), 23-26. https://doi.org/10.5750/IJPCM.V1I1.18.
Benbow, A. (2007). Mental illness, stigma, and the media. The Journal of clinical psychiatry, 68 Suppl 2, 31-5
Bensemann, C., & Watson, P. (2017). A Mental Health & Addictions service Transformation Agenda to an integrated system of care: challenges, and early successes. International Journal of Integrated Care, 17, 93. https://doi.org/10.5334/IJIC.3398.
Bergstrøm, C. (1979). The teaching social worker in family medicine: a prototype for the hospital social worker?. Social work in health care, 4 4, 409-21. https://doi.org/10.1300/J010V04N04_04.
Berkman, B., Bonander, E., Kemler, B., Rubinger, M., Rutchick, I., & Silverman, P. (1996). Social work in the academic medical center: advanced traininga necessity. Social work in health care, 24 1-2, 115-135.https://doi.org/10.1300/J010V24N01_07.
Berkman, B., Bonander, E., Rutchick, I., Silverman, P., Kemler, B., Marcus, L., & Isaacson-Rubinger, M. (1990). Social work in health care: directions in practice. Social science & medicine, 31(1), 19-26. https://doi.org/10.1016/0277-9536(90)90005-D.
Bhugra, D., & Till, A. (2013). Public mental health is about social psychiatry. International Journal of Social Psychiatry, 59, 105 - 106. https://doi.org/10.1177/0020764012464184.
Bishnoi, H., Khan, A., Avasthi, R., & , Sataveer. (2017). Community Mental Health in India: Current Scenario. International Journal of Nursing Education, 9 (3), 15-16. https://doi.org/10.5958/0974-9357.2017.00062.9.
Booysen, P., & Staniforth, B. (2017). Counselling in social work: A legitimate role?. Aotearoa New Zealand Social Work, 29 (1), 16-27. https://doi.org/10.11157/ANZSWJ-VOL29ISS1ID214.
Bowen, E., & Walton, Q. (2015). Disparities and the Social Determinants of Mental Health and Addictions: Opportunities for a Multifaceted Social Work Response. Health & Social Work, 40(3). 59 - 65. https://doi.org/10.1093/HSW/HLV034.
Braveman P, (2014). What are Health Disparities and Health Equity? We Need to Be Clear. Public Health Reports;129(1) 5-8. doi:10.1177/00333549141291S203
Bryant, L., Garnham, B., Tedmanson, D., & Diamandi, S. (2020). Social work and tele-mental health services for rural and remote communities. Advances in Telemedicine for Health Monitoring: Technologies, Design and Applications 133-147. https://doi.org/10.1049/pbhe023e_ch7.
Center for Mental Health Law and Policy. (2023). Budget Brief 2023 [PDF file]. Retrieved from https://cmhlp.org/wp-content/uploads/2023/02/Budget-Brief-2023-v3.pdf
Chappell, N. (2008). Aging and Mental Health. Social Work in Mental Health, 7, 122 - 138. https://doi.org/10.1080/15332980802072454.
Clarke, V., & Braun, V. (2017). Thematic analysis. The Journal of Positive Psychology, 12(3), 297–298. https://doi.org/10.1080/17439760.2016.1262613
Compton, M. T., & Shim, R. S. (2020). Mental Illness Prevention and Mental Health Promotion: When, Who, and How. Psychiatric Services, 71(9), 981–983. https://doi.org/10.1176/appi.ps.201900374
Corrigan, P. (1998). The impact of stigma on severe mental illness. Cognitive and Behavioral Practice, 5, 201-222. https://doi.org/10.1016/S1077-7229(98)80006-0.
Corrigan, P., Druss, B., & Perlick, D. (2014). The Impact of Mental Illness Stigma on Seeking and Participating in Mental Health Care. Psychological Science in the Public Interest, 15(3), 37 - 70. https://doi.org/10.1177/1529100614531398.
Green, D., & Ellis, S. (2017). Proactive Case Management: Social Work Active Engagement Revisited. Journal of Sociology and Social Work, 5(1), 10-16. https://doi.org/10.15640/JSSW.V5N1A2.
Dennelly, L., Sousa, C., & Roberts, K. (2021). Shaping the Future of Social Work Practice in Healthcare: Addressing COVID-19 Needs through Integrated Primary Care. Social work, 67(1), 41-47. https://doi.org/10.1093/sw/swab046.
Fairfax, C., & Feit, M. (2015). How Policy Improves Health. Social Work in Public Health, 30(5), 410 - 422. https://doi.org/10.1080/19371918.2015.1034002.
Farrer, L., Marinetti, C., Cavaco, Y., & Costongs, C. (2015). Advocacy for Health Equity: A Synthesis Review. The Milbank Quarterly, 93, 392 - 437. https://doi.org/10.1111/1468-0009.12112.
Faust, J. (2008). Clinical Social Worker as Patient Advocate in a Community Mental Health Center. Clinical Social Work Journal, 36, 293-300. https://doi.org/10.1007/S10615-007-0118-0.
Feryn, N., Corte, J., & Roose, R. (2021). The DNA of Social Work as a Partner in Primary Health Care. Social Work in Public Health, 37(5), 407 - 418. https://doi.org/10.1080/19371918.2021.2017381.
Fraher, E., Richman, E., Zerden, L., & Lombardi, B. (2018). Social Work Student and Practitioner Roles in Integrated Care Settings. American journal of preventive medicine, 54(6), S281-S289. https://doi.org/10.1016/j.amepre.2018.01.046.
Francis, A. (2014). Social Work in Mental Health: Contexts and Theories for Practice. The Sage Journal. https://doi.org/10.4135/9789351507864.
Golden, S. (2022). Disruptive Innovations to Achieve Health Equity Through Healthcare and Research Transformation. Clinical pharmacology and therapeutics, 113(3), 500-508. https://doi.org/10.1002/cpt.2812.
Gopalkrishnan, N. (2018). Cultural Diversity and Mental Health: Considerations for Policy and Practice. Frontiers in Public Health, 6, 179. https://doi.org/10.3389/fpubh.2018.00179.
Gowda, M., Das, K., Gowda, G., Karthik, K., Srinivasa, P., & Muthalayapapa, C. (2019). Founding and managing a mental health establishment under the Mental Healthcare Act 2017. Indian Journal of Psychiatry, 61, S735 - S743. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_147_19.
Gupta, S. (2021). The role of policy and legislation in mental health care. Indian Journal of Social Psychiatry, 37(2), 230 - 234. https://doi.org/10.4103/ijsp.ijsp_160_21.
Hailemariam, M., Fekadu, A., Selamu, M., Medhin, G., Prince, M., & Hanlon, C. (2016). Equitable access to integrated primary mental healthcare for people with severe mental disorders in Ethiopia: a formative study. International Journal for Equity in Health, 15, 1-10 https://doi.org/10.1186/s12939-016-0410-0.
Hamer, H., Rowe, M., & Seymour, C. (2018). ‘The right thing to do’: Fostering social inclusion for mental health service users through acts of citizenship. International Journal of Mental Health Nursing, 28(1), 297–305. https://doi.org/10.1111/inm.12533.
Hariharan, S., Krishnaprasanth, B., Stephen, T., & Aljin, V. (2020). Mental Health Scenario in India. Annals of Medical and Health Sciences Research, 10, 1058-1059.
Hashimoto, H., & Kawakami, N. (2018). Health equity. Oxford Textbook of Public Mental Health. https://doi.org/10.1093/med/9780198792994.003.0013.
Hooper, J., Saulsman, L., Hall, T., & Waters, F. (2021). Addressing the psychological impact of COVID-19 on healthcare workers: learning from a systematic review of early interventions for frontline responders. BMJ Open, 11. https://doi.org/10.1136/bmjopen-2020-044134.
Hussain, A., & Ashcroft, R. (2020). Social work leadership competencies in health and mental healthcare: a scoping review protocol. BMJ Open, 10(10). https://doi.org/10.1136/bmjopen-2020-038790.
Igbaba, S. (2023). Mental Health Promotion for Internally Displaced Persons Using Drama Therapy in Makurdi Area, North Central Nigeria. International Journal of Current Research in the Humanities, 26(1), 377-400 https://doi.org/10.4314/ijcrh.v26i1.22.
Jagannathan, A., & Reddy, S. (2021). Challenges in Social Policy Making for Psychiatric Disability in India: Lessons and Way Forward for Social Workers. British Journal of Social Work, 50(8), 2441-2451. https://doi.org/10.1093/BJSW/BCAA190.
Jayasankar, P., Nirisha, P., Manjunatha, N., Kumar, C., Gajera, G., Malathesh, B., Pandey, P., Suhas, S., Ohri, U., Kumar, R., Bajpai, P., Kumar, R., & Math, S. (2022). Are the Collaborative Video Consultations module in Diploma in Primary Care Psychiatry helpful. Indian Journal of Psychiatry, 64(3), S516 - S520. https://doi.org/10.4103/0019-5545.341490.
Jemalel, N., Barasa, M., Mmbone, C., & Ndetei, D. (2016). Efficacy of Psychoeducation on Improving Attitudes Towards Professional Psychological Help Seeking for a Mental Illness Among Teacher Trainees in Kenya. European Journal of Preventive Medicine, 4(5), 120-124. https://doi.org/10.11648/J.EJPM.20160405.13.
Jenkins, R., Kydd, R., Mullen, P., Thomson, K., Sculley, J., Kuper, S., Carroll, J., Gureje, O., Hatcher, S., Brownie, S., Carroll, C., Hollins, S., & Wong, M. (2010). International Migration of Doctors, and Its Impact on Availability of Psychiatrists in Low and Middle Income Countries. PLoS ONE, 5(2), 9049. https://doi.org/10.1371/journal.pone.0009049.
Jensen, C. (2004). Medication for Children with Attention-Deficit Hyperactivity Disorder. Clinical Social Work Journal, 32, 197-214. https://doi.org/10.1023/B:CSOW.0000024328.71427.D1.
Jones, B., & Phillips, F. (2016). Social Work and Interprofessional Education in Health Care: A Call for Continued Leadership. Journal of Social Work Education, 52(1), 18 - 29. https://doi.org/10.1080/10437797.2016.1112629.
Klos, L., Shkoliar, M., Stavkova, S., & Kokhanova, O. (2021). Social workers’ activities in the field of population’ mental health preservation in the xxi century. Wiadomości Lekarskie. Official Journal of the Polish Medical Association, 74(11), 2823-2828 https://doi.org/10.36740/wlek202111125.
Kumar, P., Jangid, P., & Sethi, S. (2018). Undergraduate psychiatry in India: A SWOT analysis. Asian journal of psychiatry, 33, 46-51. https://doi.org/10.1016/j.ajp.2018.02.018.
Levitt, A. J., Lorenzo, J., Yu, V., Wean, C., & Miller-Solarino, S. (2011). Suicide awareness and prevention workshop for social workers and paraprofessionals. Journal of Social Work Education, 47(3), 607-613.
Levy, C. (1985). NASW Code of Ethics. Social Work, 30, 451-452. https://doi.org/10.1093/SW/30.5.451.
Mahajan, P., Rajendran, P., Sunderamurthy, B., Keshavan, S., & Bazroy, J. (2019). Analyzing Indian mental health systems: Reflecting, learning, and working towards a better future. Journal of Current Research in Scientific Medicine, 5(1), 4 - 12. https://doi.org/10.4103/jcrsm.jcrsm_21_19-.
Mango, L. (2020). Health systems of underdeveloped and developing countries. International Journal of Global Health (IJGH). https://doi.org/10.14302/issn.2693-1176.ijgh-20-3489
Mann, C., Golden, J., Cronk, N., Gale, J., Hogan, T., & Washington, K. (2016). Social Workers as Behavioral Health Consultants in the Primary Care Clinic. Health & social work, 41(3), 196-200. https://doi.org/10.1093/hsw/hlw027.
Marshall-Lee, E., Hinger, C., Popovic, R., Roberts, T., & Prempeh, L. (2019). Social justice advocacy in mental health services: Consumer, community, training, and policy perspectives. Psychological services, 17(S1), 12. https://doi.org/10.1037/ser0000349.
McGorry, P., & Mei, C. (2018). Early intervention in youth mental health: progress and future directions. Evidence-Based Mental Health, 21(4), 182 - 184. https://doi.org/10.1136/ebmental-2018-300060
McLaughlin, A. (2009). Clinical Social Workers: Advocates for Social Justice. Advances in social work, 10(1), 51-68. https://doi.org/10.18060/209.
McLeod, J., & McLeod, J. (2015). Research on embedded counselling: An emerging topic of potential importance for the future of counselling psychology. Counselling Psychology Quarterly, 28(1), 27 - 43. https://doi.org/10.1080/09515070.2014.942774.
Nazar, N. (2018). The role of social workers in implementing the national concept of mental health. Social Work Education, 5(4), 45-55. https://doi.org/10.25128/2520-6230.18.4.4.
Nazar, N. (2020). The ecosystem approach in health social work. Mental Health: Global Challenges Journal, 3(2), 16-18. https://doi.org/10.32437/mhgcj.v4i2.90
Noel, L., Chen, Q., Petruzzi, L., Phillips, F., Garay, R., Valdez, C., Aranda, M., & Jones, B. (2022). Interprofessional collaboration between social workers and community health workers to address health and mental health in the United States: A systematised review. Health & social care in the community, 30(6), e6240-e6254. https://doi.org/10.1111/hsc.14061.
Okech, V., Neszméry, Š., & Mačkinová, M. (2020). Roles of social workers in mental health care teams: a systematic review of the literature. Proceedings of CBU in Social Sciences, 1, 167-172. https://doi.org/10.12955/pss.v1.66.
Okechukwu, C. (2021). A call for improved mental health workforce in low-income countries. International Journal of Social Psychiatry, 68(2), 465 - 467. https://doi.org/10.1177/00207640211039255.
Orlowski, S., Lawn, S., Matthews, B., Venning, A., Jones, G., Winsall, M., Antezana, G., Bidargaddi, N., & Musiat, P. (2017). People, processes, and systems: An observational study of the role of technology in rural youth mental health services. International Journal of Mental Health Nursing, 26(3), 259–272. https://doi.org/10.1111/inm.12262.
Pardasani, M. (2018). Teaching Students the Importance of Community Engagement and Awareness in the Areas of Mental Health and Addiction. New Directions in Treatment, Education, and Outreach for Mental Health and Addiction, 299-313. https://doi.org/10.1007/978-3-319-72778-3_20.
Peterson, A., Charles, V., Yeung, D., & Coyle, K. (2020). The Health Equity Framework: A Science- and Justice-Based Model for Public Health Researchers and Practitioners. Health Promotion Practice, 22(6), 741 - 746. https://doi.org/10.1177/1524839920950730.
Praharaj, S., Behere, R., Deora, S., & Sharma, P. (2013). Psychiatric specialization as an option for medical students in the Indian context. International Review of Psychiatry, 25(4), 419 - 424. https://doi.org/10.3109/09540261.2013.822347.
Ramsey, A., & Montgomery, K. (2014). Technology-Based Interventions in Social Work Practice: A Systematic Review of Mental Health Interventions. Social Work in Health Care, 53(9), 883 - 899. https://doi.org/10.1080/00981389.2014.925531.
Ray, S. (2022). Mental and Psychosocial Health: A Post-COVID Concern in India. Neurology India, 70(5), 2116-2120. https://doi.org/10.4103/0028-3886.359196.
Robinson, L., Dauenhauer, J., Bishop, K., & Baxter, J. (2012). Growing Health Disparities for Persons Who Are Aging With Intellectual and Developmental Disabilities: The Social Work Linchpin. Journal of Gerontological Social Work, 55(2), 175 - 190. https://doi.org/10.1080/01634372.2011.644030.
Rosenheck, R. (2012). Introduction to the special section: toward social inclusion. Psychiatric services, 63(5), 425-426. https://doi.org/10.1176/appi.ps.20120p425.
Sagar, R., & Singh, S. (2022). National Tele-Mental Health Program in India: A step towards mental health care for all? Indian journal of psychiatry, 64(2), 117-119. https://doi.org/10.4103/indianjpsychiatry.indianjpsychiatry_145_22.
Sagar-Ouriaghli, I., Godfrey, E., Bridge, L., Meade, L., & Brown, J. (2019). Improving Mental Health Service Utilization Among Men: A Systematic Review and Synthesis of Behavior Change Techniques Within Interventions Targeting Help-Seeking. American Journal of Men's Health, 13(3), 1557988319857009. https://doi.org/10.1177/1557988319857009.
Salunkhe, G., & Braeunig, M. (2019). Mental Health in India: Perspectives for Psychosomatic Medicine. An International Guide for Primary Care Setting, 343-350. https://doi.org/10.1007/978-3-030-27080-3_28.
Sawrikar, P. (2020). Service providers’ cultural self-awareness and responsible use of racial power when working with ethnic minority victims/survivors of child sexual abuse: Results from a program evaluation study in Australia. Children and Youth Services Review, 119, 105641. https://doi.org/10.1016/j.childyouth.2020.105641.
Saxena, A., & Chandrapal, S. (2021). Social Work and Policy Practice: Understanding the Role of Social Workers. British Journal of Social Work, 52(3), 1632-1642. https://doi.org/10.1093/BJSW/BCAB073.
Shanske, S., Arnold, J., Carvalho, M., & Rein, J. (2012). Social Workers as Transition Brokers: Facilitating the Transition from Paediatric to Adult Medical Care. Social Work in Health Care, 51(4), 279 - 295. https://doi.org/10.1080/00981389.2011.638419.
Sheehan, R. (2012). Forensic Social Work: A Distinctive Framework for Intervention. Social Work in Mental Health, 10(5), 409 - 425. https://doi.org/10.1080/15332985.2012.678571
Shim, R., & Starks, S. (2021). COVID-19, Structural Racism, and Mental Health Inequities: Policy Implications for an Emerging Syndemic. Psychiatric services, 72(10), 1193-1198. https://doi.org/10.1176/appi.ps.202000725.
Shrivastava, S., Shrivastava, P., & Ramasamy, J. (2014). Medical social worker: Strengthening linkages between the hospital and the community. International Journal of Health System and Disaster Management, 2(02), 130. https://doi.org/10.4103/2347-9019.139074.
Singh, A., Chopra, M., Singh, R, S., (2023). Assessment of Effective uptake of Telemanas Service in India. EPRA International Journal of Multidisciplinary Research (IJMR), 9(7), 20-26. http://www.eprajournals.net/index.php/IJMR/article/view/2343
Stewart, T. (2014). Undocumented Immigrants and Policy Advocacy: Reasserting the Activist Roots of Social Work. Columbia Social Work Review, 12(1) , 33-42. https://doi.org/10.7916/D8FB527C.Sussman, S., Kattari, S., Baezconde-Garbanati, L., & Glackin, S. (2020). Commentary: The Problems of Grouping All Adversity into a Special Populations Label. Evaluation & the Health Professions, 43(1), 66 - 70. https://doi.org/10.1177/0163278719882738.
Taylor-Rodgers, E., & Batterham, P. (2014). Evaluation of an online psychoeducation intervention to promote mental health help seeking attitudes and intentions among young adults: randomised controlled trial. Journal of affective disorders, 168, 65-71. https://doi.org/10.1016/j.jad.2014.06.047.
TNN (2023, April 1). Nimhans takes psychiatric healthcare to doorstep in Bengaluru. Times of India [PDF File] Retrieved from https://timesofindia.indiatimes.com/city/bengaluru/nimhans-takes-psychiatric-healthcare-to-doorstep-in-bengaluru/articleshow/90483444.cms
Stanhope, V., Videka, L., Thirning, H., & McKay, M. (2015). Moving toward integrated health: An opportunity for social work. Social Work in Health Care, 54(5), 383-407. DOI: 10.1080/00981389.2015.1025122.
Villatoro, A., Mays, V., Ponce, N., & Aneshensel, C. (2018). Perceived Need for Mental Health Care: The Intersection of Race, Ethnicity, Gender, and Socioeconomic Status. Society and Mental Health, 8(1), 1 - 24. https://doi.org/10.1177/2156869317718889.
Wagle, K., Cottingham, A., Butler, D., Grover, J., & Litzelman, D. (2021). Understanding social workers’ hidden roles in medication safety for older adults: A qualitative study. Social Work in Health Care, 60(4), 369 - 386. https://doi.org/10.1080/00981389.2021.1900023.
Weng, S. (2021). Ethics in integrated health care: social workers’ perspective. Ethics & Behavior, 32(3), 259 - 272. https://doi.org/10.1080/10508422.2021.1883431.
Wilkinson, G., Sager, A., Selig, S., Antonelli, R., Morton, S., Hirsch, G., Lee, C., Ortiz, A., Fox, D., Lupi, M., Acuff, C., & Wachman, M. (2017). No Equity, No Triple A Strategic Proposals to Advance Health Equity in a Volatile Policy Environment. American Journal of Public Health, 107(S3), S223-S228. https://doi.org/10.2105/AJPH.2017.304000.
Winkelmann, G. (2016). Social work in health – The way ahead. Aotearoa New Zealand Social Work, 25(4), 85-88. https://doi.org/10.11157/ANZSWJ-VOL25ISS4ID66.
Woerner, C. (2015). Serviço Social e Saúde Mental: atuação do assistente social em comunidade terapêutica / Social Work and Mental Health: practice of the social worker in a social therapeutic community. Textos & Contextos (Porto Alegre), 14(1), 174-185. https://doi.org/10.15448/1677-9509.2015.1.18155.
Yip, K. (2000). The community care movement in mental health services: Implications for social work practice. International Social Work, 43(1), 33 - 48. https://doi.org/10.1177/A010519.
Author´s
Address:
Chandramathi Ramaswamy
Department of Social work
Bharathiar University, Coimbatore
+91 94878-04414
chandramathiramaswamy@gmail.com
Author´s
Address:
Revanth R
Research Scholar, Department of Social work
Bharathiar University, Coimbatore
revanthajay1@gmail.com
Author´s
Address:
Jagadeesh R
Research Scholar, Department of Social work
Bharathiar University, Coimbatore
jprjagadeesh@gmail.com
Author´s
Address:
Tamilarasu Sampath
Research Scholar, Department of Sociology and Population studies
Bharathiar University, Coimbatore
tamilarasu.dsps@buc.edu.in
Author´s
Address:
Dr. F. X. Lovelina Little Flower
Department of Social work
Bharathiar University, Coimbatore
lovelina@buc.edu.in