Ensuring Equity in Health Services in Hospital Settings through Social Work Interventions: A Mixed Method Study
Md. Golam Azam, University of Dhaka
Muhammad Mamunur Rashid, Shaikh Burhanuddin Post Graduate College
Md. Abdul Mazid, University of Dhaka
Abstract & Keywords: The study aimed to explore the status of equity in health service provisions and the process of ensuring equity in health services in the Social Welfare Department (SWD) of a tertiary care hospital with the application and effectiveness of social work interventions at micro and macro levels. Under pragmatism, the study employed a mixed-method approach within the explorative research framework that applied social surveys, case studies, and observations. A total of 120 poor diabetic patients for a survey, 10 patients for case studies, and 10 key informants were chosen for the study. The key findings reveal that SWD equitably distributes healthcare services through the identification of patients, assessment of psychophysical conditions, economic and social conditions, and distribution of services to the patients. The need-based and rehabilitation-based social work interventions at micro and macro levels contributed to the patients getting satisfied with the healthcare services in the hospital. In conclusion, the tertiary care services for poor diabetic patients need to be upgraded to meet their healthcare needs.
Keywords: Health Equity; Health Services; Tertiary Hospital; Social Work Interventions; Micro-Macro Level; Poor Patients of Bangladesh
1 Introduction
Bangladesh is a low-income country situated in South Asia near the bank of the Bay of Bengal surrounded by India from three sides and Myanmar from the East. The population of the country is 169.8 million 68.34% live in rural areas and the rest of 31.66% live in urban areas (Bangladesh Bureau of Statistics (BBS), 2023). In the hospital settings, the country has only 9.9 doctors, nurses, and midwives per 10000 people which is much lower than the global median of 48.6 (Ministry of Health and Family Welfare (MOHFW) Bangladesh & World Health Organization (WHO) Bangladesh, 2021). In Bangladesh, nearly 13% of treatment seekers use government health services, 27% people use private/NGO services and the rest of 60% of the people use unqualified health services (Cockcroft et al., 2004; Directorate General of Health Services (DGHS), 2018). Mannan (2013) also found that women and the poor are mostly found to use public health facilities and physical accessibility of public health services is not a barrier anymore, but social and economic accessibility remains a major hurdle in this sector (Mannan, 2013). A study by Siddiqui et al., (2007) revealed that the quality of services in private hospitals scored higher than that of public hospitals for nursing care, tangible hospital matters such as cleanliness, supply of utilities, and availability of drugs (Siddiqui et al., 2007). Although theoretically, Bangladesh has sophisticated health facilities open for all, only a few are utilizing these services due to factors like geographical location, position, social class, power, and wealth. A large number of underserved populations are mainly from the rural and urban poor and marginalized segments of people (Bangladesh Health Watch (BHW), 2007, 2008; Mannan, 2013). Werner, (2009) argued that free public-health services for the urban and rural poor exist theoretically in Bangladesh but the poor are largely excluded from the public facilities. The only cause is a lack of money (for gifts or bribes) or connections with service providers (Werner, 2009). The overall condition of health benefits in the richest group is better than the poorest group. The rich population is free from urban-rural and richest-poorest health disparities than the poor people (Mamunur Rashid et al., 2019). The Social Welfare Departments (SWDs) of different tertiary care hospitals are providing various types of social work interventions in Bangladesh, although the nature and quality of social services are different. The concept of diabetes and social services to poor diabetic patients by a tertiary care hospital have been discussed including a review of literature on the equity in health service in hospital settings and social work interventions. Methodology, sampling, data collection methods, and data analysis process have also been presented. Also, the demographic, social, economic, and health profile of the patients, the state of health services and equity in health, the process of ensuring equity and health, and, the application of social work interventions have been explored in the study. The results and recommendations within the policy framework have also been addressed.
2 Conceptual and theoretical discussions
In this section, the researchers discuss the concepts of equity in health, diabetes, social services to poor diabetic patients, and also the theoretical perspectives. Health equity was defined by the American Centers for Disease Control and Prevention (CDC) as “Health equity is the state in which everyone has a fair and just opportunity to attain their highest level of health” (Centers for Disease Control and Prevention (CDC), 2023). To attain health equity uninterrupted societal initiatives and assistance are essential for addressing the past and contemporary inequalities. It is required to overcome economic, social, and other barriers to health, the healthcare system, and facilities. By abolishing avoidable health inequalities health equity can be attained (Braveman et al., 2017; Centers for Disease Control and Prevention (CDC), 2023); (Office of Disease Prevention and Health Promotion (ODPHP), 2021). According to the World Health Organization (WHO), “Health equity is achieved when everyone can attain their full potential for health and well-being” (World Health Organization (WHO), 2023). It is also marked as the nonexistence of systematic inequities in health and social aspects (determinants) of the health of those people who live in various tiers of social hierarchy (Whitehead, 1992; Zere et al., 2013). Zere et al., (2013) recommend three key steps for measuring equity in health and these steps are to: (a) identify the degrees of interest of the persons whose needs should be measured; (b) measure the socio-economic stage of the persons for classifying the households, families, and individuals into diverse social and economic layers; and, (c) measure the degrees of inequalities in the society (Zere et al., 2013). In this study, equity in health means equal access to and equal benefits of health for all, especially weaker segments of the people who are vulnerable economically and socially and are living in diverse social and economic tiers.
In terms of conceptual clarification, the Centers for Disease Control and Prevention (CDC) described “diabetes is a chronic (long-lasting) health condition that affects how your body turns food into energy” (Centers for Disease Control and Prevention, 2022). World Health Organization (WHO) describes two conditions for diabetes such as “the pancreas does not produce enough insulin” or “the body cannot effectively use the insulin it produces” (World Health Organization, 2016). According to Alam et al., (2021) “Diabetes mellitus… results from a complex interaction of genetic and environmental factors, principally characterized by hyperglycemia, polyuria, and polyphagia” (p.35). Diabetes can create several complications in the human body including heart attack, stroke, failure of kidney activities, leg amputation, vision loss, and nervous system damage (World Health Organization, 2016). Diabetes-related complications can lead to a variety of disabling, life-threatening, and expensive complications, including cardiovascular events (Nativel et al., 2018) like stroke, heart attack, renal disease, neuropathy, peripheral arterial disease (PAD), lower-limb adverse events, and visual impairment (Deshpande et al., 2008; Nativel et al., 2018; Shariful Islam et al., 2013; Soyoye et al., 2021).
Here in the paper, the poor diabetic patients are those who are living at or below the poverty line experiencing multiple diseases, and failing to manage treatment costs and daily necessities. In Bangladesh, millions of people are diagnosed with diabetes (Diabetic Association of Bangladesh - BADAS, 2023). Since 1956, Bangladesh Diabetes Somity (BADAS) has been providing treatment facilities and other support services to the diabetic patients of Bangladesh. It provides services through a tertiary care hospital and other satellite centers (Diabetic Association of Bangladesh -BADAS, 2023). The Statistical Yearbook 2020-2021 of BADAS shows that till 30 June 2020, the registered number of diabetic patients was 6,44,782 and the Social Welfare Department (SWD) of that tertiary care hospital specialized in diabetes provided various services to the 74,001 poor diabetic patients. For indoor and outdoor patients, DSW renders services such as drug supply to non-paying patients, blood collection for the patients, and eye lenses, and black optics to eye operation patients (Diabetic Association of Bangladesh - BADAS, 2023). Moreover, the hospital provides some welfare services like taking socioeconomic history, socioeconomic and psycho-social diagnosis, and aiding insulin and drugs to indoor and outdoor patients.
From the theoretical point of view, American Philosopher John Rawls’s social justice theory is applied to identify the key areas of health-related issues and injustice in Hospital settings (Rawls, 1971). In this study, the researchers focused on Rawls’s theory of “equity of opportunity” for ensuring social justice in hospital settings and then on Norman Daniel’s approach, as Daniel extended Rawls’s theory into the areas of public health (Shafique et al., 2018). The study also covers approaches like health in the list of primary social goods (Coogan, 2007), and (b) Norman Daniel’s normal function approach (Daniels, 2009; Ekmekci & Arda, 2015). Theories of social justice are silent in the cases of health, health equity is addressed limitedly and the focus is only on healthcare (Daniels, 1985; Fried, 1975; Peter & Evans, 2001). Rawls described the concept of “justice as fairness” in his book ‘A Theory of Justice’ (Rawls, 1971), and his theory demands prioritizing the “worst off group” in society, especially the poorest segment of the people in society (Marchand et al., 1998; Peter & Evans, 2001). To ensure equitable distribution, Rawls's idea of “original position” where no one knows anything about their position in society (Rawls, 1971). The position was termed as blank state and the situation is termed as “a veil of ignorance” (Rawls, 1971). The concept of the “veil of ignorance” for formulating a set of principles for society to keep the social functioning smooth without unfairness to anyone (Rawls, 1971). The veil prevents the individuals from remembering about their own “concept of good” and their “life plans” (Rawls, 2005). The main point of Rawls's theory is that rational individuals fix the “principles of justice” by giving priority to the “worst off behind” the “veil of ignorance”, where people are unacquainted with their personal belongings (Peter & Evans, 2001). Extending Rawls, (1993) suggestion Peter and Evans claimed that “Inequalities in health are unjust if they are caused by unjust social arrangements” (Peter & Evans, 2001). Norman Daniel extended Rawls’s theory of justice arguing that justice is a very necessary obligation to public health (Daniels, 2001), and he also prioritized the moral significance of health, so that it can contribute implicitly to the introduction of a variety of opportunities for the mass people. Daniel also advocates that the government and other stakeholders should take policy initiatives for equalizing and distributing life opportunities such as elementary education, and reasonable housing to reduce health inequities (Daniels, 2001).
Within the framework of John Rawl’s social justice theory, the Social Welfare Department (SWD) and the tertiary care hospital collaboratively provide healthcare services including assessment of biopsychic disorders and socioeconomic status, care planning and interventions, psychotherapy and counseling, medication management, follow-ups, and rehabilitation support services facilitating to promote health equity and ensuring justice to reduce inequalities.
3 Review of literature
Many research scholars have conducted research studies on equity in health in hospital settings across the countries. However, in the context of health equity in Bangladesh, an insignificant number of studies were found in Science Direct, MDPI, Google Scholar, and PubMed. So far literature survey indicates that no studies on social work interventions on diabetic care were observed in hospital settings in Bangladesh, but a few research articles on healthcare issues in tertiary hospitals have been found in the literature. In a study conducted by O’Donnell et al., (2007) the distribution of public healthcare is pro-rich for most of the developing countries in the world (O’Donnell et al., 2007). According to a study by Khan et al., (2017), an overall pro-rich distribution of healthcare benefits was observed in the study, and healthcare benefits from private providers were seen to favor the richer socioeconomic groups. The public and NGO providers have shown little inequity (Khan et al., 2017). Khan et al., (2017) also found that about 95.9% of inequity had been shown by the private providers of service to overall inequity. The poorest socioeconomic group contains 21.8% of the need for healthcare received only 12.7% of the benefits, while the richest group with 18.0% of the need accounted for 32.8% of the health benefits (Khan et al., 2017). A study in China on older adults aged 65 or older found that most of the districts in the city center have better access to tertiary healthcare facilities than the suburban or peripheral districts (Chen et al., 2022). The study also identified that equity of access to tertiary hospitals was better for the senior population than the total number of populations (Chen et al., 2022).
A study in Australia on After-Hours Social Work Service in a tertiary care hospital revealed that social work service providers provided service to patients in the Emergency Department (ED) and Intensive Care Unit (ICU) where counseling for trauma, grief, and distress were mainly provided (Pereira et al., 2017). McLaughlin, (2015) indicated that hospital social workers are given high value by service users for their responsiveness, emotional support, and practical help during the process of hospitalization in Northern Ireland. Another study in Australia on the social work interventions in six tertiary care hospitals revealed that residential location, socio-economic status, gender, relationship status, responsibilities for dependent children, and other complex individual circumstances were key reasons for referral to social workers (Pockett et al., 2020, 2022). In these hospitals, social workers applied multiple social work interventions across multiple systems and a few key intervention tools are psycho-social assessment, financial management, counseling and education, service coordination, and advocacy (Pockett et al., 2020, 2022). A study on social work in the Department of Military Hospital by Beder, (2009) found that social workers mentioned cognitive-behavioral, solution-focused, and strengths-based theoretical orientations. Moreover, eye movement desensitization and reprocessing (EMDR) was also used by social workers (Beder, 2009). Social workers also applied several intervention techniques such as cognitive behavioral theory (CBT), Solution-focused brief therapy (SFBT), and Strengths-based practice (Beder, 2009).
Nam et al., (2023) in their study in Vietnam observed that most of the hospitals in the study implemented social work services during the medical examination and treatment processes, health education and communication services, resource mobilization and coordination services, and health worker support services (Nam et al., 2023). The study also showed that central and provincial hospitals provided social work services better than the district hospitals and, pediatric (tertiary) hospitals were seen to provide better social work services than the general hospitals for children in Vietnam (Nam et al., 2023). Fraher et al., (2018) in their study identified 29 activities of social work students and practitioners' role in integrated care settings. The study identified most frequently performed functions such as employing cultural competency (95%), engaging in patient electronic health records (90%), social determinants of health (88%), team-based care (88%), patient education (83%), provide informal consultations (76%), care management (73%), risk stratification (67%), medications management (50%), problem-solving therapy (43%), behavioral activation (38%) and, functional assessment of daily living skills (33%) (Fraher et al., 2018).
Social work interventions for diabetic patients are a neglected area of intervention and Decoster (2005) argued that social workers have enormous potential to improve the lives of diabetic patients by applying their intervention roles as educators, advocates, counselors, therapists, resource brokers, and community developers. At the early intervention level, social workers employed the roles of educator, resource broker, change agent for clients; counselor; advocate, and community change agent (Agiri, 2019). Ciporen (2012) emphasized providing meaningful interventions for lifestyle changes for diabetic-2 children including combining individual, family, group, and outreach medical education modalities along with the provisions of food stamps (Ciporen, 2012). Rane and Gåfvels (2017) developed a psychosocial treatment plan with clear goals for each patient newly diagnosed with type-1 and type-2 diabetes in Sweden and applied a few social work interventions like counseling, problem-focused support, social information, and advice (Rane & Gåfvels, 2017). Aceves et al. (2022) applied five social care activities including awareness, adjustment, assistance, advocacy, and alignment for the National Diabetic Treatment Guidelines.
From the above literature review, it can be said that no studies were found on ensuring equity in health services in tertiary hospital settings through the application of social work interventions and the effectiveness of these intervention methods in Bangladesh. So, there is a certain level of knowledge gap in this regard and intensive research studies are imperative in this field, particularly in the context of ensuring equity in health through the application of social work interventions in Bangladesh.
4 Objectives of the study
The study was designed to explore the status of equity in health service provisions and the process of ensuring equity in health services in the Social Welfare Department (SWD) of a tertiary care hospital with the application of social work interventions and their effectiveness at micro and macro levels. This study aimed to know the status of health services and equity in health, understand the process of ensuring equity in health by application of social work intervention approaches at micro and macro levels and explore the ways of promoting the quality of services rendered to diabetic patients within the framework of pragmatic welfare policies.
5 Methodology of the study
5.1 Population of the study
The study population (respondents) were poor diabetic patients admitted to a tertiary care hospital who received services and benefits from the Social Welfare Department under the Ministry of Social Welfare. Each of the diabetic patients receiving hospital care services was considered the unit of the study.
5.2 Sampling procedure and sample
The study followed a mixed-method design that combined quantitative and qualitative methods of data collection. To collect quantitative data,120 diabetic patients were chosen for the sample survey by using a convenience sampling procedure from the patients admitted to the tertiary care center. During the study period, the population size was found to be smaller than we expected in the hospital. So, taking the issue of short stay, availability, and accessibility to some admitted patients during the study period a small size of diabetic patients (120) was selected for the study. To collect in-depth qualitative data by using case studies and key informants interviews a purposive sampling procedure was applied. In the case of collecting information (in words/texts), ten (10) beneficiaries (diabetic patients) were selected purposively for in-depth case interviews. Ten (10) key informants were interviewed to get their opinions, views, and insights about the existing process of providing services and the use of social work intervention approaches.
5.3 Research approach and method
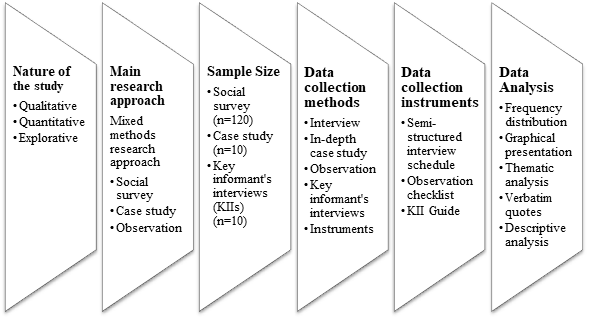
Under pragmatism (a research paradigm), the study followed a mixed-method approach and was conducted within an explorative research framework. In the study, both quantitative and qualitative methods of investigation were employed, and qualitative and quantitative data collection techniques were also applied to gather quantitative (numerical) data as well as qualitative (in-depth descriptive/narrative) information/data. The rationale for using the mixed method approach/design of the study is to find out the quantitative data on health service provisions (with demographic, socio-economic, and health profiles of the patients) in the hospital under study, and also the qualitative information (about diabetes and socio-economic, psychophysical health challenges experienced by the diabetic patients). The qualitative data/information was thematically categorized by giving labels and values (in numerical form) that reflect the coding process. For instance, the effectiveness of social work interventions as a qualitative variable has been categorized by using a Likert-like scale that provides a coherent interpretation of the themes/variables. In the study, the state of health services and equity in health, the process of ensuring equity in health, and the ways of promoting the quality of services rendered to diabetic patients are explored within the framework of pragmatic social welfare policies.
5.4 Data collection methods and instruments
To collect quantitative data, the social survey method was employed using a semi-structured interview schedule (self-administered questionnaire). To gather qualitative data on the variables set for the investigation, an in-depth case interview guide, observation checklist, and key informant’s interview guide were also applied. Data collection instruments were prepared both in the indigenous/local language (Bengali) and in English. Instruments in English were only used for interviewing key informants who were educated and could speak in English. The diabetic patients and social work service providers in the hospital setting were contacted to collect both quantitative and qualitative data. Particularly, data in the form of talks, discussions, conversations, and interviews were also collected. In doing so, audio-visual devices to record data were used in data collection. Data collection was carried out between June 01, 2022, to February 15, 2023.
5.5 Data analysis
As the study followed a combination of qualitative and quantitative methods of data collection, the collected data were analyzed by using descriptive statistics such as mean, standard deviation, and frequency percentage. In addition, qualitative data were processed by using thematic analysis, verbatim quotes, and narrative discussions.
Figure 1: Methodology of the study
5.6 Ethical considerations
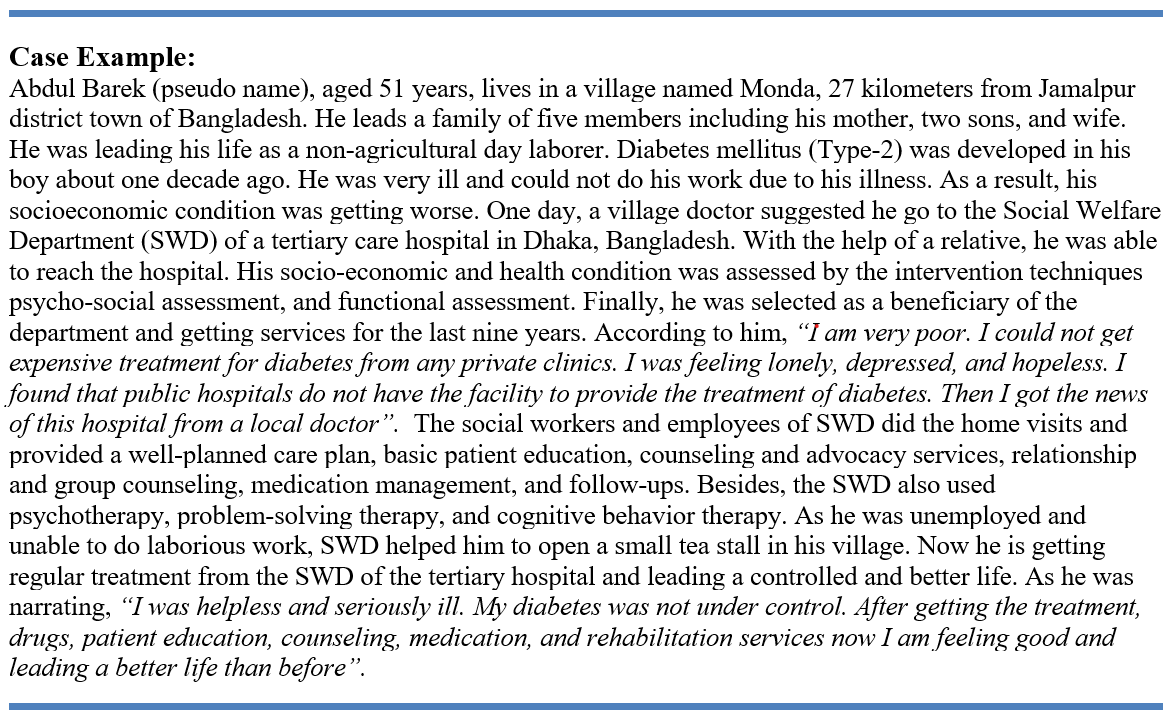
As data were collected from the beneficiaries of the Social Welfare Department (SWD) of the tertiary care hospital, permission was obtained from the authority of the SWD. Respondents were informed about the objectives of the study and informed consent was taken before conducting the interviews. In discussions and interviews, the researcher took verbal consent from respondents/participants for note-taking and recording information. To maintain privacy, the names and personal identities of the respondents were changed (converted to pseudo names) when reporting case studies and other private issues of individual respondents. Within the legal frame of the nation and hospital rules and regulations, data collection, and data maintenance within normative practice in the hospital setting have been strictly maintained.
6 Findings of the study
6.1 Demographic, social, economic, and health profile of the patients
The distribution of the different social and economic characteristics of poor diabetic patients is presented below:
Table 1: Demographic, social, and economic variables of the respondents
Demographic, social, and economic variables (Number of frequencies, N=120)
|
Demographic, social, and economic variables |
Responses (frequencies) |
Percentage (%) |
|
|
Gender |
Male |
38 |
31.67 |
|
Female |
82 |
68.33 |
|
|
Age (in years) |
20-30 |
8 |
6.67 |
|
30-40 |
18 |
15 |
|
|
40-50 |
58 |
48.33 |
|
|
50-60 |
20 |
16.67 |
|
|
60-70 |
14 |
11.67 |
|
|
70-80 |
2 |
1.67 |
|
|
Marital Status |
Married |
74 |
61.67 |
|
Unmarried |
8 |
6.67 |
|
|
Widow/widower |
12 |
10.0 |
|
|
Divorced due to diabetes |
14 |
11.67 |
|
|
Separated due to diabetes |
12 |
10.0 |
|
|
Educational Status |
Illiterate |
72 |
60.0 |
|
Primary level (Class 1-5) |
24 |
20.0 |
|
|
Secondary level (Class 6-10) |
16 |
13.33 |
|
|
Higher Secondary level (Class 11-12) |
4 |
3.33 |
|
|
Graduate/Post-Graduate |
4 |
3.33 |
|
|
Knowledge about diabetes |
Have no knowledge |
98 |
81.67 |
|
Have knowledge |
22 |
18.33 |
|
|
Occupation |
Farmer/Day laborer |
8 |
6.67 |
|
Housewife |
72 |
60.0 |
|
|
Housemaid |
10 |
8.33 |
|
|
Dependent |
28 |
23.33 |
|
|
Beggary |
2 |
1.67 |
|
|
Monthly income (BDT) |
0-5,000 |
10 |
8.33 |
|
5,000-10,000 |
42 |
35.00 |
|
|
10,000-15,000 |
44 |
36.67 |
|
|
15,000-20,000 |
18 |
15.00 |
|
|
20,000-25,000 |
4 |
3.33 |
|
|
25,000-30,000 |
2 |
1.67 |
|
Table 1 shows that 68.33% of beneficiary respondents are female and the rest are male. It was observed that most of the beneficiaries were female in this tertiary care hospital. According to an officer of SWD (pseudo name):
“The prevalence of diabetes is higher among females than males due to their food habits, physical labor, and other bio-physical causes” (Kabir, personal communication, September 10, 2022).
The age distribution of the study indicates that the highest number of respondents (48.33%) belong to the age group 40-50, whereas 16.67% and 11.67% of respondents are from the age group 50-60 and 60-70 years respectively. Even findings also show that 6.67% are suffering from diabetes aged below 30 years. The mean age of the respondents was found to be 46.67 (±10.87). Regarding marital status, 61.67% are married. Of the respondents, 11.67% were found divorced, and another 10% were separated due to diabetes complications. According to a female respondent (pseudo name):
“I had to accept a divorce letter from my ex-husband due to diabetes and related physical illness. My husband did not want to bear my treatment expenses” (Rubina, M., personal communication, October 19, 2022).
Table 1 also shows that 60% of respondents are illiterate and only 20% have completed the primary level of education. The majority number of respondents 81.67%) did not know about diabetes. Among the beneficiaries, 60% were housewives, and 8.33% worked as housemaids. About 28% of respondents are dependent on others like the elderly, and persons with disabilities (PWDs). The prevalence of diabetes was found low (6.67%) among the farmers and day laborers. The majority of the respondents (95%) family income was less than BDT 20,000 (160 USD) per month and the highest number of respondents (36.67%) family income was in the income group of BDT 10000-15,000 (80-120 USD, 1$=125 BDT) per month. Another 35% of respondents hold the income group of BDT 5000-10,000 (40-80 USD). The average family income of the respondents is BDT 11,250 (90 USD).
Table 2: Diabetes and related bio-psychosocial and economic challenges
|
Types of Diabetes |
Frequency and Percentage (%) |
Socio-economic Problems Due to Diabetes |
Frequency and Percentage (%) |
Psychological Challenges |
Frequency and Percentage (%) |
Suffered from related diseases |
Frequency and Percentage (%) |
|
DM (Type-1) |
22 (18.33%) |
Financial crisis |
120 (100%) |
No psychological challenges |
18 (15%) |
No other biological diseases |
22 (18.33%) |
|
DM (Type-2) |
94 (78.33%) |
Relationship problem |
74 (61.67%) |
Emotional problems and a sense of isolation |
94 (78.33%) |
Cardiac problems |
42 (35%) |
|
Gestational diabetes |
2 (1.67%) |
Shelter problems |
6 (5%) |
Anxiety, panic, feeling a loss of desire to live |
64 (53.33%) |
Eye Damage |
34 (28.33%) |
|
Others |
2 (1.67%) |
Medicare problems |
114 (95%) |
Nervousness and fear of insanity, death |
4 (3.33%) |
Chronic Kidney Diseases, CKD |
42 (35 %) |
|
|
|
Divorced due to diabetes |
14 (11.67%) |
The feeling of helplessness, hopelessness, loneliness, sadness, or guilt |
102 (85%) |
Others |
18 (15%) |
|
|
|
Separated due to diabetes |
12 (10%) |
Depression, eating disorders |
78 (65%) |
|
|
|
|
|
Others |
42 (35%) |
Others |
6 (5%) |
|
|
|
Total |
120 (100%) |
|
120 (Multiple Response) |
|
120 (Multiple Response) |
|
120 (Multiple Response) |
Table 2 reveals that among 120 diabetic patients, 78.33% are suffering from Diabetes Mellitus (DM) Type -2, and the rest are suffering from DM Type-1, a very insignificant number (1.67%) are suffering from Gestational diabetes. The respondents are suffering from socioeconomic problems caused by diabetes and 100% are suffering from economic crises, 74% from relationship problems, and 95% from Medicare problems. Concerning psychological challenges, 78.33% feel emotional problems and have a sense of isolation, 85% feel helplessness, loneliness, sadness, frightened, or guilt, 65% experience depression with eating disorders, and 53.33% feel anxiety, panic, and a loss of desire to live. Patients with diabetes are also affected by other diabetes-related diseases like cardiac problems (35%), eyesight damage (28.33%), and chronic kidney diseases -CKD (35%). According to a respondent (pseudo name):
“I am 61 years old… suffering from diabetes for the last nine years with problems of eye vision, and heart diseases. My physical condition is getting worse, and I also feel frustrated with losing the desire to live” (Ramjan, M., personal communication, October 28, 2022).
6.2 State of health services and equity in health
The Social Welfare Department in the tertiary hospital under study provides various types of need-based and rehabilitation-based services (preventive, curative, and rehabilitative) to all patients of diverse socioeconomic classes. The health services for the patients are shown in the Table 3:
Table 3: Health services and benefits received by the patients (beneficiaries)
|
Health Services/benefits |
Number of beneficiaries (N=120) |
Percentage (%) |
|
Need-Based Services |
||
|
Biopsychic assessment (medical) |
120 |
100 |
|
Socioeconomic assessment (social and economic) |
120 |
100 |
|
Follow-up services |
120 |
100 |
|
Home visits |
115 |
95.83 |
|
Training and education on diabetes |
120 |
100 |
|
Hospitalization of patients |
120 |
100 |
|
Support assistance in urgent admission to the hospital |
37 |
30.83 |
|
Supply of insulin |
120 |
100 |
|
Free medication |
120 |
100 |
|
Investigation of patients |
120 |
100 |
|
Long-term care service |
95 |
79.17 |
|
Rehabilitation Based Services |
||
|
Advocacy and counseling services |
120 |
100 |
|
Connecting with support services |
45 |
37.5 |
|
Providing lenses for patients with vision problems |
11 |
9.17 |
|
Providing wheelchairs to disabled patients |
07 |
5.83 |
|
Economic assistance for the rehabilitation of poor |
24 |
20 |
|
Employment generation for unemployed patients |
15 |
12.5 |
It was found in Table 3 that 100% of patients received need-based services like biopsychic assessment, socioeconomic assessment, follow-up services, training and education on diabetes, hospitalization of patients, supply of insulin, free medication, and investigation of patients. Besides, 95.83% of patients received home visit services from social workers, and 79.17% of patients received long-term care services. On the contrary, the patients also received rehabilitation services from the Social Welfare Department (SWD). Among 120 respondents, 100% received advocacy and counseling services, and 37.5% were given connections to support services. Another 20% received economic assistance as a rehabilitation-based service. The study reveals that most of the services are free of cost and some provisions are distributed according to the socioeconomic condition, social status, and level of poverty to ensure proper justice, fairness, and equity. Services are distributed free of cost (fully free), 25% free, 50% free, and 75% free according to the needs of poor diabetic patients. An officer of SWD narrated (pseudo name):
“We provide services to diabetic patients who are from poor and marginalized communities. We distribute our services by receiving minimum fees or free of cost. Socioeconomic conditions of the patients are considered to ensure justice and equity” (Akhter, F., personal communication, October 29, 2022).
A social worker (pseudo name) narrated the equity in the service provision of the hospital as:
“We value the people; we care and provide services to poor and marginalized patients. We do not discriminate the patients based on economic status, education, social class, religion, or ethnicity. We want to ensure biopsychosocial well-being for the patients through our services” (Islam, R., personal communication, November 02, 2022).
6.3 The process of ensuring equity in health
The tertiary care hospital maintains a process of selecting poor diabetic patients to ensure equity in health by applying social work interventions at micro and macro levels. The process of ensuring equity in health is shown in the figure 2:
Figure 2: Process of ensuring equity in health through social work interventions

The Social Welfare Department (SWD) of the hospital selects the beneficiaries of services according to the bio-psychic, social, and economic conditions of the patients. The department prioritizes patients who are insulin-dependent, suffering from diabetes-related diseases, living in poor socioeconomic conditions, physically challenged, destitute and vagabond, and have low income and expenditure. Social workers of SWD follow a process for selecting the beneficiaries that includes providing a case history date, case history, and psychosocial study, diagnosis of the problem, psychosocial treatment, referral or counseling, home visits for the crosschecking (confirmation of information), follow-up, and assessment. Then SWD workers apply micro-level social work interventions to diabetic patients and their family members, and macro-level social work interventions to the social groups, communities, institutes, and society as a whole. Social workers intervene in some targeted areas such as physical health, psychological health, family relationships, person-in-environment, socioeconomic condition, poverty, and poor physical conditions, food habits and lifestyle, health education and training, and so on. All interventions are undertaken to achieve goals like equity in health and justice in the health and well-being of the pro-poor, physically challenged, and marginalized diabetic patients. The process of selecting beneficiaries was narrated by a junior social welfare officer (pseudo name):
“After having the case history of the admitted patients, we ensure suitability for their services through psychosocial study and home visits. We provide them with psychosocial treatment and need-based and rehabilitation-based interventions and services for a long time” (Sheikh, A., personal communication, January 13, 2023).
6.4 Effectiveness of social work interventions applied at micro and macro levels
The study observed that diabetic patients and their family members and caregivers received different types of services from the Social Welfare Department (SWD) of the tertiary care hospital.
Table 4: Occasion of taking services from the Social Welfare Department (SWD)
|
Occasion of service with diabetic patients |
Occasion of contact with family members, caregivers, and others |
||||
|
Number of Contacts |
Frequency, N=120 |
Percentage |
Number of Contacts |
Frequency, N=120 |
Percentage |
|
1-3 times |
31 |
25.83 |
1-3 times |
39 |
32.5 |
|
4-6 times |
39 |
32.5 |
4-6 times |
26 |
21.67 |
|
7-9 times |
27 |
22.5 |
7-9 times |
14 |
11.67 |
|
10-12 times + |
23 |
19.17 |
10-12 times + |
9 |
7.5 |
|
Total |
120 |
100 |
Total |
88 |
73.33 |
|
|
|
|
Missing |
32 |
26.67 |
Table 4 shows that 25.83% of the diabetic patients received 1-3 times, 32.5% received 4-6 times and 22.5% received 7-9 times of services. Moreover, 19.17% of beneficiaries received 10 to more than 12 times of services from the SWD. Social workers of SWD contacted 73.33% of family members and caregivers of diabetic patients. Among them 32.5% received 1-3 times, 21.67% received 4-6 times, and 11.67% received 7-9 times of services, training, and guidelines. Only 7.5% of them received 10 to more than 12 times of contacts and guidelines.
The hospital social workers of the tertiary care hospital had to deal with the challenges of patients with diabetes and related diseases. Because of the variations of patients in terms of bio-psychic and socioeconomic conditions, social workers applied different social work interventions to handle the challenges at the micro and macro levels of the patient’s environment. The intervention methods and intervention process are shown in the following Table 5.
Table 5: Social work intervention methods applied at micro and macro levels
Figure 3: Effectiveness of social work interventions applied at micro and macro levels
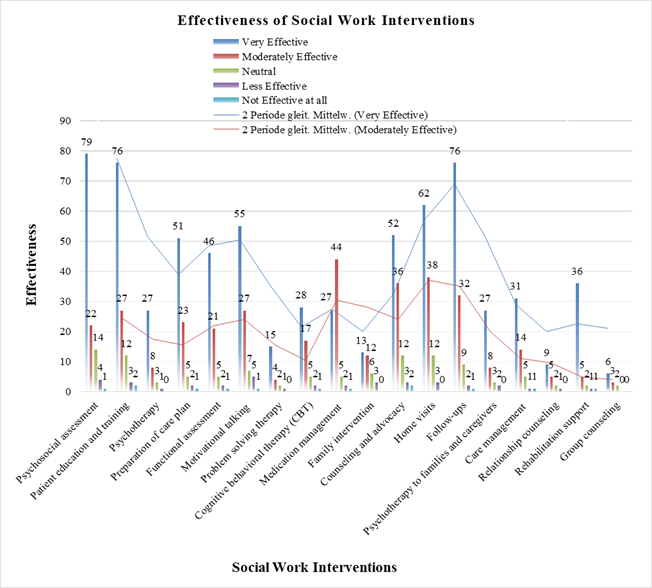
In the above figure, the effectiveness is calculated by summing up the very effective and moderately effective percentage of each intervention techniques. Figure 3 highlights that in terms of psychotherapy, psychotherapy to family members and caregivers, preparation of care plan, medication management, follow-ups, and rehabilitation support social work interventions showed 90% to 92% effectiveness and, care management, home visits, counseling and advocacy, functional assessment, motivational talking, patient education, PST, CBT, relationship counseling, and group counseling showed 80% to 89 % effectiveness. Besides, psychosocial assessment and family intervention also showed 70% to 79% effectiveness according to the analysis of the data. Overall, the social work interventions applied in the tertiary care hospital indicate better effectiveness.
7 Discussions of the study findings
The findings of the study indicate that most of the beneficiaries of the SWD of the tertiary care hospital are female. Most of the female diabetics are housewives. The highest number of diabetic patients belongs to the 40-50 years of age group, even people less than 30 years old are also found to suffer from diabetes. Most of the beneficiaries are illiterate and only one-fifth of them completed primary education. The average family income of the respondents is BDT 11,250 as they belong to poor socio-economic status. The study also reveals that the highest number of patients (78.33%) are suffering from DM (type-2) and others are suffering from DM (type-1) (18.33%) and gestational diabetes. Chowdhury et al., (2022) also support the findings that the prevalence of diabetes was observed and is increasing alarmingly day by day. Most of the diabetic patients are suffering from socioeconomic problems like financial crises, Medicare problems, relationship problems, and divorce and separation because of diabetes. On the contrary, psychological challenges like emotional problems, a sense of isolation, anxiety, panic, feelings of helplessness, and loneliness are very common among diabetic patients. Leone et al., (2012) also support the psychological impacts like depression associated with diabetes are linked to their lower social and economic status. A good number of patients were also found to suffer from cardiac problems, eyesight damage, chronic kidney diseases (CKD), and other diseases. The SWD of the tertiary care hospital was found to provide various need-based (i.e. bio-psychic assessment, socioeconomic assessment, follow-up service, training and education, supply of insulin, free medication, investigation, long-term care) and rehabilitation-based services (i.e. advocacy and counseling services, economic assistance, employment generation) for fully free of cost or by a small amount of money according to the socioeconomic conditions and needs of the poor diabetic patients for ensuring equity in health. In line with the demands of John Rawl’s social justice theory and concept of ‘equity of opportunity’, the study findings showed that SWD of the studied tertiary hospital prioritized the ‘worst off groups’ in the society, especially the poorest segments of the population. The findings of the study by Fraher et al., (2018) also support the findings of the present study to some extent. The study revealed that the highest number of beneficiaries (diabetic patients) received 4-6 times services and a substantial number of beneficiaries received 1-3 times, 7-9 times, and 10- more than 12 times of services from the SWD. Moreover, 73% of family members and caregivers were also in contact with the interventions applied by SWD.
The current study also explored that 100% of respondents were intervened by using micro-level social work intervention methods like psycho-social assessment, patients’ education and training, and follow-ups. Apart from that, other intervention techniques such as psychotherapy, home visits, problem-solving therapy, counseling and advocacy, and medication management were also applied to a large number of patients. Macro social work interventions such as psychotherapy for families and caregivers, care management, relationship counseling, group counseling, and rehabilitation support were applied. Findings showed that most of the social work interventions were found very effective (73% to 92% effective). Psychotherapy, psychotherapy to family members and caregivers, preparation of care plan, medication management, follow-ups, and rehabilitation support social work interventions showed 90% to 92% effectiveness, and, care management, home visits, counseling and advocacy, functional assessment, motivational talking, patient education, PST, CBT, relationship counseling, and group counseling showed 80% to 89 % effectiveness. Besides, psychosocial assessment and family intervention also showed 73% to 79% effectiveness according to the analysis of the data. Overall, the intervention techniques at micro and macro levels have shown better effectiveness for ensuring equity and justice in healthcare service provisions. Pockett et al., (2022) in their study showed that social workers played a very significant role in the provision of effective psychosocial care to the patients in the tertiary hospital. The findings by Nam et al., (2023) pediatric tertiary hospitals, and central and provincial hospitals have shown a better trend in providing social work services in Vietnam. The findings regarding interventions and provision of welfare services by DSW are in line with the argument of Norman Daniel that justice is a very necessary obligation to public health (Daniels, 2001) and the moral significance of health that results in a variety of opportunities for the mass people.
8 Conclusions and recommendations
The study followed a mixed method approach and tried to focus on ensuring equity in health services in hospital settings through social work interventions, effective application of social work intervention approaches to deal with diabetic cases, promoting the quality of services being rendered to diabetic patients within the framework of pragmatic social welfare policies. From the study findings, it can be concluded that most of the patients are female and housewives with poor socioeconomic backgrounds. The majority of the patients were found to suffer from DM (type 2) along with other physical and mental health problems. Based on need-based and rehabilitation-based social work intervention methods used by the SWD at micro and macro levels were found to be more effective for the patients. So far as the study tried to explore equity in healthcare services, the results showed positive outcomes in terms of access to health services, health justice, health rights, and fair distribution of welfare services. In terms of promoting quality care services for poor diabetic patients, available and adequate care services with proper medication, counseling services, and psychotherapy within the application of hospital-based social work, clinical social work, gerontological and geriatric social work, social casework, and social group work need to be promoted and ensured in practice. In addition, a pragmatic and sustainable health care and service policy for diabetic patients should be formulated and brought into effective practice for the well-being of poor diabetic patients. And tertiary care services need to be upgraded to meet the healthcare service needs of the patients. The study suggests further research studies to be undertaken for those who are interested in the areas of healthcare service promotion in tertiary care hospital settings in Bangladesh.
References:
Aceves, B., Gunn, R., Pisciotta, M., Razon, N., Cottrell, E., Hessler, D., Gold, R., & Gottlieb, L. M. (2022). Social Care Recommendations in National Diabetes Treatment Guidelines. Current diabetes reports, 22(10), 481–491. https://doi.org/10.1007/s11892-022-01490-z
Agiri, R. (2019). Social Workers and Early Intervention with Diabetic Clients (Publication No. 6876) [Doctoral dissertation, Walden University]. Walden Dissertations and Doctoral Studies. https://scholarworks.waldenu.edu/dissertations/6876/
Alam, S., Hasan, Md. K., Neaz, S., Hussain, N., Hossain, Md. F., & Rahman, T. (2021). Diabetes Mellitus: Insights from Epidemiology, Biochemistry, Risk Factors, Diagnosis, Complications and Comprehensive Management. Diabetology 2021, Vol. 2, Pages 36-50, 2(2), 36–50. https://doi.org/10.3390/DIABETOLOGY2020004
Bangladesh Bureau of Statistics (BBS). (2023). Population and Housing Census 2022: Post Enumeration Check (PEC) Adjusted Population. http://www.bbs.gov.bd/site/page/47856ad0-7e1c-4aab-bd78-892733bc06eb/Population-and-Housing-Census
Bangladesh Health Watch (BHW). (2007). Sate of Health in Bangladesh (2006): Challenges of Achieving Equity in Health. https://app.bangladeshhealthwatch.org/docs/reports_pdf/bhw-reports/the-state-of-health-in-bangladesh-2006-1642949432.pdf
Bangladesh Health Watch (BHW). (2008). Health Workforce in Bangladesh: Who constitutes the Healthcare System?. https://app.bangladeshhealthwatch.org/docs/reports_pdf/bhw-reports/the-state-of-health-in-bangladesh-2007-1643179723.pdf
Beder, J. (2009). Social Work in the Department of Defense Hospital: Impact, Role, and Interventions. Military Medicine, 174(5), 486–490. https://doi.org/10.7205/MILMED-D-03-9908
Braveman, P., Arkine, E., Orleans, T., Proctor, D., & Plough, A. (2017). What Is Health Equity? And What Difference Does a Definition Make? https://www.rwjf.org/en/library/research/2017/05/what-is-health-equity-.html
Ciporen, H. (2012). Social Workers’ Role in Combating the New Epidemic of Type 2 Diabetes in Children: Clinical Interventions at the Hall Family Center for Pediatric Endocrinology and Diabetes. Social Work in Health Care, 51(1), 22–35. https://doi.org/10.1080/00981389.2011.622634
Centers for Disease Control and Prevention (CDC). (2023). What is Health Equity? Centers for Disease Control and Prevention. https://www.cdc.gov/healthequity/whatis/index.html
Centers for Disease Control and Prevention (CDC). (2022, June 20). The Facts, Stats, and Impacts of Diabetes. https://www.cdc.gov/diabetes/library/spotlights/diabetes-facts-stats.html
Chen, Y., Ding, Q., & Shen, Y. (2022). Assessing Accessibility and Social Equity of Tertiary Hospitals for Older Adults: A City-Wide Study of Tianjin, China. Buildings 2022, 12(12), 2107. https://doi.org/10.3390/BUILDINGS12122107
Chowdhury, M. A. B., Islam, M., Rahman, J., Uddin, M. J., & Haque, M. R. (2022). Diabetes among adults in Bangladesh: changes in prevalence and risk factors between two cross-sectional surveys. BMJ Open, 12(8). https://doi.org/10.1136/BMJOPEN-2021-055044
Cockcroft, A., Milne, D., & Andersson, N. (2004). Bangladesh Health and Population Sector Programme, 1998-2003: the third service delivery survey, 2003: final report, annexes. (No Title).
Coogan, E. H. (2007). Rawls and Health Care [Honors Thesis. Paper 501, Colby College]. https://digitalcommons.colby.edu/honorstheses/501
Daniels, N. (1985). Just Health Care. In Studies in Philosophy and Health Policy. Cambridge University Press. https://doi.org/DOI: 10.1017/CBO9780511624971
Daniels, N. (2001). Justice, Health, and Healthcare. The American Journal of Bioethics, 1(2), 2–16. https://doi.org/https://doi.org/10.1162/152651601300168834
Daniels, N. (2009). Just Health: Meeting Health Needs Fairly. Cambridge University Press.
Decoster, V. A. (2005). Challenges of type 2 diabetes and the role of health care social work: a neglected area of practice. In Social work diagnosis in contemporary practice (pp. 395-406). USA: Oxford University Press.
Deshpande, A. D., Harris-Hayes, M., & Schootman, M. (2008). Epidemiology of Diabetes and Diabetes-Related Complications. Physical Therapy, 88(11), 1254. https://doi.org/10.2522/PTJ.20080020
Diabetic Association of Bangladesh - BADAS. (2023). Statistical Yearbook 2020-2021. https://www.dab-bd.org/publication.php
Directorate General of Health Services (DGHS). (2018). Health Bulletin 2018. https://old.dghs.gov.bd/images/docs/Publicaations/HB%202018%20final.pdf
Ekmekci, P. E., & Arda, B. (2015). Enhancing John Rawls’s theory of justice to cover health and social determinants of health. Acta Bioethica, 21, 227–236.
Fraher, E. P., Richman, E. L., Zerden, L. de S., & Lombardi, B. (2018). Social Work Student and Practitioner Roles in Integrated Care Settings. American Journal of Preventive Medicine, 54(6), S281–S289. https://doi.org/10.1016/J.AMEPRE.2018.01.046
Fried, C. (1975). Rights and Health Care — Beyond Equity and Efficiency. New England Journal of Medicine, 293(5), 241–245. https://doi.org/10.1056/NEJM197507312930507
Khan, J. A. M., Ahmed, S., MacLennan, M., Sarker, A. R., Sultana, M., & Rahman, H. (2017). Benefit incidence analysis of healthcare in Bangladesh - Equity matters for universal health coverage. Health Policy and Planning, 32(3), 359–365. https://doi.org/10.1093/heapol/czw131
Leone, T., Coast, E., Narayanan, S., & de Graft Aikins, A. (2012). Diabetes and depression comorbidity and socio-economic status in low and middle income countries (LMICs): a mapping of the evidence. Globalization and Health, 8(1), 39. https://doi.org/10.1186/1744-8603-8-39
Mamunur Rashid, Md., Roy, T. K., & Singh, B. P. (2019). Socioeconomic Health Disparities in Bangladesh through Lorenz Curve and Gini Ratio: Evidence from BDHS Survey. International Journal of Statistics and Analysis, 9(1), 11. https://doi.org/10.37622/ijsa/9.1.2019.11-23
Mannan, M. A. (2013). Access to Public Health Facilities in Bangladesh: A Study on Facility Utilisation and Burden of Treatment. Bangladesh Development Studies, XXXVI(4). https://bids.org.bd/uploads/publication/BDS/36/36-4/2_Mannan.pdf
Marchand, S., Wikler, D., & Landesman, B. (1998). Class, Health, and Justice. The Milbank Quarterly, 76(3), 449–467. https://doi.org/https://doi.org/10.1111/1468-0009.00098
McLaughlin, J. (2015). Social work in acute hospital settings in Northern Ireland: The views of service users, carers and multi-disciplinary professionals. Journal of Social Work, 16(2), 135–154. https://doi.org/10.1177/1468017314568843
Ministry of Health and Family Welfare (MOHFW) Bangladesh, & World Health Organization (WHO) Bangladesh. (2021). Assessment of Healthcare Providers in Bangladesh 2021. https://cdn.who.int/media/docs/default-source/searo/bangladesh/assessment-of-healthcare-providers-in-bangladesh-2021.pdf
Nam, P. T., Dung, N. H., Hung, N. T., Thu, L. T., Thuy, N. T. B., Trung, N. Van, Ly, D. K. K., Thi Phuong, N., Trang, P. T., Oanh, L. T. M., & Liem, N. K. (2023). Social Work Services for Children at Vietnam’s Hospitals: A Qualitative Study. Journal of Social Service Research, 49(1), 42–53. https://doi.org/10.1080/01488376.2022.2156971
Nativel, M., Potier, L., Alexandre, L., Baillet-Blanco, L., Ducasse, E., Velho, G., Marre, M., Roussel, R., Rigalleau, V., & Mohammedi, K. (2018). Lower extremity arterial disease in patients with diabetes: a contemporary narrative review. Cardiovascular Diabetology 2018 17:1, 17(1), 1–14. https://doi.org/10.1186/S12933-018-0781-1
O’Donnell, O., van Doorslaer, E., Rannan-Eliya, R. P., Somanathan, A., Adhikari, S. R., Harbianto, D., Garg, C. C., Hanvoravongchai, P., Huq, M. N., Karan, A., Leung, G. M., Ng, C. W., Pande, B. R., Tin, K., Tisayaticom, K., Trisnantoro, L., Zhang, Y., & Zhao, Y. (2007). The incidence of public spending on healthcare: Comparative evidence from Asia. World Bank Economic Review, 21(1), 93–123. https://doi.org/10.1093/WBER/LHL009
Office of Disease Prevention and Health Promotion (ODPHP). (2021, August). Healthy People 2020: Disparities. U.S. Department of Health and Human Services. https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities
Pereira, M., Wire, G., & Stiller, K. (2017). A Retrospective Review of the After-Hours Social Work Service in a Tertiary-Care Public Hospital in Australia. Internet Journal of Allied Health Sciences and Practice, 15(1), 1. https://doi.org/10.46743/1540-580X/2017.1613
Peter, F., & Evans, T. (2001). Ethical Dimensions of Health Equity. In Timothy Evans, Margaret Whitehead, Finn Diderichsen, Abbas Bhuiya, & Meg Wirth (Eds.), Challenging Inequities in Health: From Ethics to Action (pp. 24–33). Oxford University Press. https://doi.org/https://doi.org/10.1093/acprof:oso/9780195137408.003.0003
Pockett, R., Hobbs, K., Araullo, R., & Dave, K. (2020). Social Work Interventions in Cancer Care: Final Report. https://doi.org/10.25910/5e49ba7193967
Pockett, R., Hobbs, K., Araullo, R., & Dave, K. (2022). Social Work Interventions in Cancer Care. Australian Social Work, 75(2), 137–151. https://doi.org/10.1080/0312407X.2020.1748673
Rane, K., & Gåfvels, C. (2017). Social work interventions in Sweden for patients newly diagnosed with type 1 or type 2 diabetes. Social Work in Health Care, 56(8), 700–713. https://doi.org/10.1080/00981389.2017.1331948
Rawls, J. (1971). A theory of justice (Original Edition). Harvard University Press.
Rawls, J. (1993). The law of peoples. In S. Shute & S. Hurley (Eds.), On Human Rights: The Oxford Amnesty Lectures (pp. 41–82). Basic Books.
Rawls, J. (2005). A theory of justice (Original Edition). Cambridge University Press.
Shafique, S., Bhattacharyya, D. S., Anwar, I., & Adams, A. (2018). Right to health and social justice in Bangladesh: Ethical dilemmas and obligations of state and non-state actors to ensure health for urban poor. BMC Medical Ethics, 19. https://doi.org/10.1186/s12910-018-0285-2
Shariful Islam, S. M., Lechner, A., Ferrari, U., Froeschl, G., Niessen, L. W., Seissler, J., & Alam, D. S. (2013). Social and economic impact of diabetics in Bangladesh: Protocol for a case-control study. BMC Public Health, 13(1), 1–9. https://doi.org/10.1186/1471-2458-13-1217/PEER-REVIEW
Siddiqui, N., Khandaker, S. A., Shahjahan, M., & Khandaker, A. (2007). Comparison of Services of Public, Private and Foreign Hospitals from the Perspective of Bangladeshi Patients. J HEALTH POPUL NUTR, 25(2), 221–230.
Soyoye, D. O., Abiodun, O. O., Ikem, R. T., Kolawole, B. A., & Akintomide, A. O. (2021). Diabetes and peripheral artery disease: A review. World Journal of Diabetes, 12(6), 827. https://doi.org/10.4239/WJD.V12.I6.827
Werner, W. J. (2009). Micro-insurance in Bangladesh: risk protection for the poor? Journal of Health, Population, and Nutrition, 27(4), 563–573. https://doi.org/10.3329/JHPN.V27I4.3402
Whitehead M. (1992). The concepts and principles of equity and health. International Journal of Health Services: Planning, Administration, Evaluation, 22(3), 429–445. https://doi.org/10.2190/986L-LHQ6-2VTE-YRRN
World Health Organization. (2016). Global report on diabetes. World Health Organization. https://www.who.int/publications/i/item/9789241565257
World Health Organization (WHO). (2023). Health Equity. World Health Organization. https://www.who.int/health-topics/health-equity#tab=tab_1
Zere, E., Suehiro, Y., Arifeen, A., Moonesinghe, L., Chanda, S. K., & Kirigia, J. M. (2013). Equity in reproductive and maternal health services in Bangladesh. International Journal for Equity in Health, 12(90), 1–8. http://www.equityhealthj.com/content/12/1/90
Author´s
Address:
Md. Golam Azam, Ph.D.
Professor, Institute of Social Welfare and Research, University of Dhaka
37-F, North Fuller Road, Dhaka University Campus, Dhaka-1000, Bangladesh Adress
+880-1912-238343
g.azam2011@gmail.com; golamazam@du.ac.bd
Author´s
Address:
Muhammad Mamunur Rashid
Shaikh Burhanuddin Post Graduate College
62, Nazimuddin Road, Dhaka-1100, Bangladesh Adress
+880-1521-555866
mamunhm94@gmail.com
Author´s
Address:
Md. Abdul Mazid
Institute of Social Welfare and Research, University of Dhaka
Flat: 4-A, 90/1, Crescent Road, Kalabagan, Dhaka-1205, Bangladesh
+880-1753-266292
mazid.abdul_1994@yahoo.com